AI technology is being used to further improve a ground-breaking scheme that has already helped to transform the care of patients with chronic respiratory illness across Hull and East Yorkshire.
Since implementing the original scheme March 2023, we have seen a 40% reduction in the number of patients with COPD (Chronic Obstructive Pulmonary Disease) needing to come back into hospital for treatment.
This is one of only two such services in the UK and now it is hoped that the use of Artificial Intelligence could help us to reduce this even further – possibly by as much as 90%.
Professor of Respiratory Medicine, Mike Crooks, who runs the service, said: “By using the Lenus COPD support system, we are able to treat COPD patients using virtual wards – so they can remain in the comfort of their own home.
“One of the characteristics of the condition is that people are prone to worsening of their symptoms that often results in needing hospital treatment but using the app can help to prevent this, by keeping track of how patients are feeling and what their symptoms are.
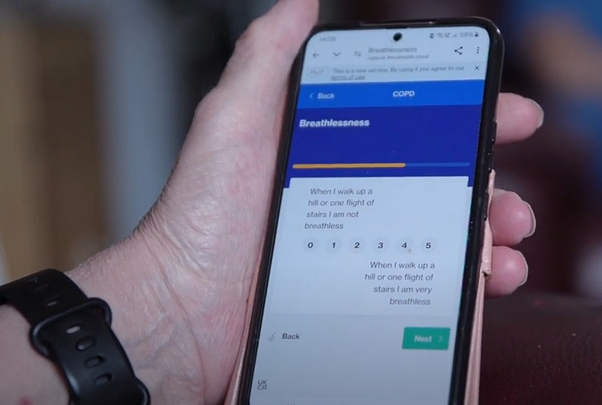
“The patients use a version of the app that prompts them on a daily, weekly, and monthly basis to answer questions about their wellbeing and their symptoms and all that data is compiled together and put onto the clinician app. Patients can also message our team directly.
“This encourages them to self-monitor their symptoms so they understand their condition better, what’s normal for them in terms of day-today variation and prompts them to make contact to initiate treatment early, so that we can give them the care they need to get them back on the right path before the point they need to come into hospital.
“This has already had a significant impact on reducing the number of patients who get to the stage where they need hospital care.
“The next phase will be to use AI to analyse this data and help us to identify trends and triggers that are likely to result in COPD patients requiring care and put interventions in place to support them before they reach this point.”
Ruth, who was diagnosed with COPD at the age of 40, has been using the Lenus app as part of her treatment. She said: “Before the Lenus, I was using the hospital three or four times a year and now those visits have been cut down to virtually zero.
“If I need to reach out to a clinician, I know that the app’s there and I can do that.”
Marcia Rankin-Smith, Project Delivery Lead at Lenus Health, added: “Through our work with Humber Health Partnership, we have been able to gather real-world evidence demonstrating that providing Lenus digital tools for COPD care in deprived areas reduces hospital admissions and lowers costs of care. The in-year cost savings evidenced by the project will be particularly important to strengthen the business case for continued investment.
“Beyond the positive clinical and economic impact, we have fostered a remarkably strong working relationship with the Respiratory Team in Hull. Their expertise and insights have been key to improving the service, and we are thrilled to share our success story with the broader healthcare community.”













 Her partner died of a brain haemorrhage in 1999 and she transferred to surgical wards on the sixth floor of Hull Royal Infirmary, moving closer to the hospital so she could walk to work. At the same time, she converted her SEN registration to qualify as a State Registered Nurse after two years of studying at university.
Her partner died of a brain haemorrhage in 1999 and she transferred to surgical wards on the sixth floor of Hull Royal Infirmary, moving closer to the hospital so she could walk to work. At the same time, she converted her SEN registration to qualify as a State Registered Nurse after two years of studying at university.








