Patients with brain tumours are to benefit from precision surgery after Hull’s team of neurosurgeons secured a £100,000 investment to upgrade technology.
NHS Humber Health Partnership has invested £100,000 in digital software to enable neurosurgeons to conduct brain surgery with pinpoint accuracy, reducing the risk of damage to key functions like speech, vision and movement.
The neurosurgery team, based in the Neurosciences Unit at Hull Royal Infirmary, will now be able offer safer and more effective treatment to patients with brain tumours or aneurysms using the Elements software by medical technology company Brainlab.
 Consultant Neurosurgeon Chittoor Rajaraman said: “For the first time in Hull, we will be able to use this technology to offer patients safer surgery, with better outcomes.
Consultant Neurosurgeon Chittoor Rajaraman said: “For the first time in Hull, we will be able to use this technology to offer patients safer surgery, with better outcomes.
“Hull is keeping pace with developments in neurosurgery so, although we are a smaller unit compared to other parts of the country, our patients are receiving the best possible treatment delivered by the latest technological advances.”
Hull Royal Infirmary’s neurosurgeons treat around 80 patients a year with cancerous brain tumours called Glioblastoma (GB). Although the most common type of malignant brain tumour, Glioblastoma is incurable and grows rapidly. Surgery aims to give patients the best quality of life for as long as possible and neurosurgeons attempt to remove the tumour from the brain, known as resection.
However, this type of brain surgery carries high risk of damage to important parts of the brain such as those used to control movements, speech or vision because of their proximity to the tumour. “Brain shift” can also occur during surgery, rendering scans taken before the patient is in theatre less accurate.
Hull is one of over 15 neurosurgery units around the country, including King’s College, Oxford and Imperial College in London, which have been taking part in a national surgical trial known as FUTURE-GB for the past four years.
More than 300 patients are being monitored over two stages to see what difference a combination of new technology makes to post-surgery recovery, quality of life and survival.
Based on their experience in the trial using the latest software, Mr Rajaraman and his team have secured funding over five years to pay for the new Elements software, enabling neurosurgeons to plan each step of surgery to map and remove as much of the tumour as possible.
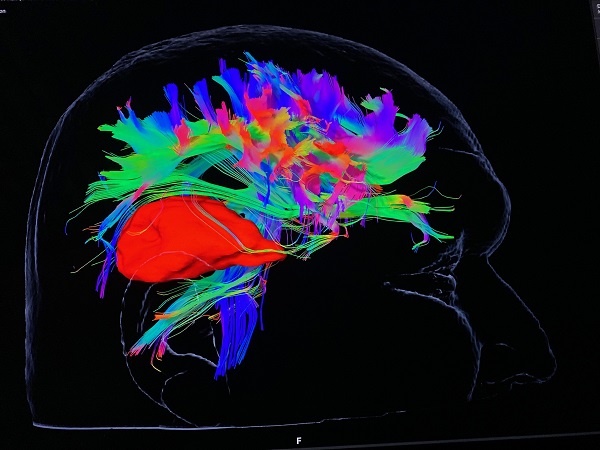
Real-time ultrasound imaging is produced during surgery, providing the neurosurgeon with on-the-spot information to help them adapt or change course if brain shift has occurred to protect key “wiring” in the brain as it can combine with the tractography images of the Brainlab Elements software.
Intra-operative ultrasound helps to reduce the time patients spend in theatre as the neurosurgery team will no longer have to halt the already-complex surgery to send the patient for an MRI scan to check the progress of the resection.

Mr Rajaraman said: “We can request ultrasound scans within a minute or two and then carry on, without the need to stop surgery for a patient to have an MRI.
“It is much better for the patient, achieving better outcomes and a greater quality of life for as long as possible.”