National ODP Day highlights the incredible work of some of the NHS’s true unsung heroes
They’re some of the true unsung heroes of the Covid pandemic, but ask the average person on the street what an Operating Department Practictioner (ODP) is and most people wouldn’t even know.
Highly trained to assist in all aspects of surgical theatre, many ODPs were taken away from their normal duties in 2020 and the early months of 2021 to swell the Covid workforce.
They left roles they knew like the back of their hand to work on unfamiliar wards, to help nurse the sick and dying, and to share the load with their fellow colleagues.
But today, Friday 14th May, is National ODP Day, an opportunity for us to shine a light on the scores of ODPs working across Hull Royal Infirmary (HRI) and Castle Hill Hospital and show what an amazing, multi-skilled bunch they are.
“For many people, the route to becoming an ODP isn’t always a direct or straightforward one”, says Gill MacLeod, Charge Nurse for Hull University Teaching Hospitals NHS Trust.
“We have ODPs in our trust who have come to the role having started out in very different careers; a porter, for example, a chef, and even someone who studied zoology at university!

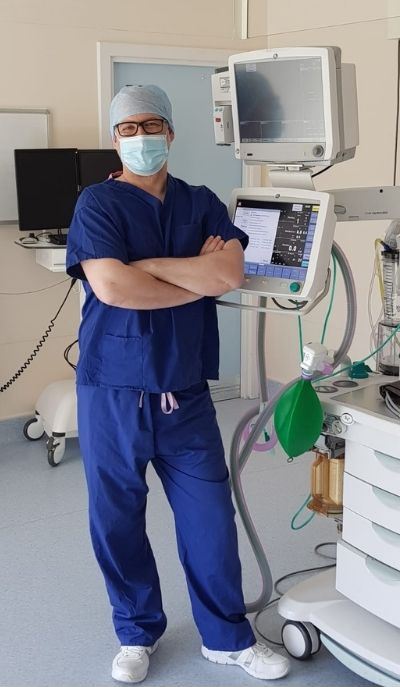
Operating Department Practitioner, Matt Appleyard
“As they are most usually found supporting in surgical theatres, ODPs can often go ‘unseen’ and so it’s not always the most obvious of NHS career choices, but ODPs are a vital part of the clinical team, providing valuable, professional expertise during a patient’s stay in hospital.”
ODP duties are split into three main areas;
- Anaesthetics, which involves assessing the patient before surgery, safely preparing drugs and other anaesthetic equipment, and monitoring the patient throughout their operation
- Scrub, which sees them preparing the theatre, supporting the surgeon during operations and acting as the patient’s advocate
- Recovery, which involves monitoring the patient after surgery to ensure they are stable and progressing well
Although ODPs are employed within operating theatres first and foremost, thanks to the Covid pandemic, they are increasingly being recognised for their skills in other areas, such as intensive care and emergency care.
Normally seen working across HRI’s main theatres, Matt Appleyard (pictured, right) is one ODP who was redeployed last year as the number of planned operations fell and the need for help was felt more acutely on the trust’s Covid wards.
“My role completely changed during the pandemic,” he says.
“I was redeployed to the Covid high dependency ward for six months, which was emotionally and mentally challenging. This work involved looking after extremely ill patients who needed ventilation and high flow oxygen.
“As an ODP, we don’t normally get ward experience so I had to use transferable skills, working alongside my ward colleagues, to observe their practice and ensure patients continued to be well supported. While it was outside my comfort zone to start, I feel this has definitely made me a better practitioner; it’s improved my emotional intelligence, enabled me to better understand different parts of the hospital, and ultimately it’s helped me to improve the direct care I provide to patients.
“The learning opportunities and the sheer variety of work involved in the ODP role are really what make it so interesting and so rewarding; one day I could find myself in a team helping to remove a brain tumour, the next could be on labour ward for a Caesarean section!”
Alex Macleod, ODP at Castle Hill Hospital
Originally a hospital porter who went on to qualify as an ODP (then known as an Operating Department Assistant) in 1993, Alex MacLeod (left) works in Breast, ENT and Plastics theatres at Castle Hill. He too was among those who stepped up to support Covid patients in their hour of need:
“During the first wave, I was responsible for preparing six extra ICU bays which could be used for patients needing ventilation.
“Then during the second wave I was redeployed to Ward 100 at Hull Royal, which was being used as a Covid ward. It was difficult because it was so different to my usual scope of practice, but I appreciated the unprecedented situation everybody was in and did my best to embrace the challenge, transferring my existing skill set to help however I could.
“While it was obviously a terrible time for everybody, I tried to view it was a positive experience and I was just really glad we could help.”
For more information about the work of Operating Department Practitioners and to find out if this is the career for you, visit the NHS Careers website.





 Emma Smith, Head of Discharge Liaison Services at the trust, said: “This new system means patients will get the very best care in the most appropriate place for them because they will no longer be kept in hospital once they are well enough to leave.
Emma Smith, Head of Discharge Liaison Services at the trust, said: “This new system means patients will get the very best care in the most appropriate place for them because they will no longer be kept in hospital once they are well enough to leave. New guidance and funding has been introduced by the Government to speed up the process and remove some of the barriers involved in discharging patients efficiently from hospital.
New guidance and funding has been introduced by the Government to speed up the process and remove some of the barriers involved in discharging patients efficiently from hospital.


 Ward Sister Hayley Butler said her entire team, including nursing staff, housekeeper and hygienist, ward clerks, cleaning staff and caterers as well as members of the multi-disciplinary team looking after patients, stepped up to the challenge.
Ward Sister Hayley Butler said her entire team, including nursing staff, housekeeper and hygienist, ward clerks, cleaning staff and caterers as well as members of the multi-disciplinary team looking after patients, stepped up to the challenge.
 Priyai Parkinson, Research Delivery Lead at Hull University Teaching Hospitals NHS Trust, said: “We are looking for volunteers to take part in a study to see what happens in the immune system when a second (boost) dose of Covid-19 vaccine is a different type to the first.
Priyai Parkinson, Research Delivery Lead at Hull University Teaching Hospitals NHS Trust, said: “We are looking for volunteers to take part in a study to see what happens in the immune system when a second (boost) dose of Covid-19 vaccine is a different type to the first. Adult volunteers of 50 years and older who have received one dose of either the Pfizer or AstraZeneca vaccine in the last eight to 12 weeks are being invited to take part in this latest trial, led by the Oxford Vaccine Group, part of the University of Oxford.
Adult volunteers of 50 years and older who have received one dose of either the Pfizer or AstraZeneca vaccine in the last eight to 12 weeks are being invited to take part in this latest trial, led by the Oxford Vaccine Group, part of the University of Oxford.

 Women attending scans to check on the growth of their baby throughout their pregnancy will also be able to bring their partner or another adult from today.
Women attending scans to check on the growth of their baby throughout their pregnancy will also be able to bring their partner or another adult from today.