The role of the hospital pharmacist can often be misunderstood, but the recent coronavirus pandemic has really given Hull University Teaching Hospitals’ pharmacy team the chance to shine.
Comprising more than 180 staff working across Hull Royal Infirmary and Castle Hill Hospital, the team has carried out many essential ‘behind-the-scenes’ duties which have allowed doctors and nurses to continue their life-saving work.
As well as ensuring a consistent on-going supply of medications for both COVID and non-COVID patients in recent weeks, the team has also played a key role in research and development to better understand and tackle the disease, whilst also supporting front-line care.
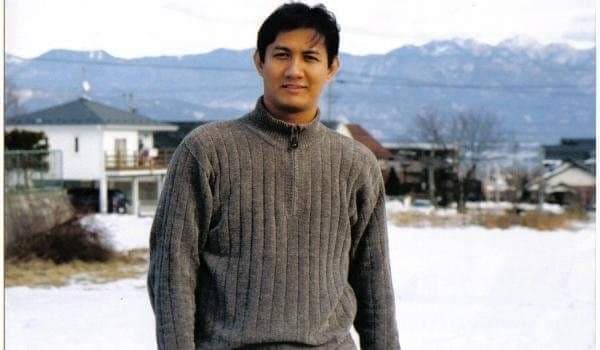
Paul O’Brien, Deputy Chief Pharmacist at the trust explains:

Members of the Pharmacy Procurement Team
“As the coronavirus situation began to escalate, one of the main concerns we had as a trust was obtaining essential medications which would be needed to treat coronavirus, especially in intensive care, such as sedatives and muscle relaxants. Demand for these types of drugs was high, particularly in parts of the UK such as London and Birmingham which were seeing significantly higher numbers of cases than we were in Hull at the start.
“Our pharmacy procurement team worked alongside other NHS trusts, as part of a national network, to ensure supply and demand was managed. In some cases, because of supply issues, the drugs that we would normally use had to be changed for alternatives, so this would mean working with our clinicians to approve the change, developing a new protocol for their use, and arranging refrigeration if the new drugs required temperature control. We’d then need to follow up with staff, making sure they were aware of the substitutions and felt fully supported in their use. It wasn’t unusual, therefore, for our clinical pharmacy teams to be donning full PPE and spending time on wards and intensive care units alongside staff and COVID positive patients to oversee their medicines management.
“Managing the daily checklist of critical medications was no mean feat. Some of the drugs we needed had to be sourced from Europe and the United States, which meant the names and strengths could all be different to the UK versions. Our procurement team worked with our IM&T colleagues to develop an algorithm which ensured, no matter how the drug came in, we were confident and secure in our supply.
“I’m really proud of the fact that, with their hard work and a lot of careful planning, working together across the country, we haven’t run out of supplies of any of our critical medications at any point during the pandemic.
Paul continues:
“At times like this, when a new virus is emerging, there is always a strong focus on research and development to better understand it and to try and find ways of treating patients or protecting society against the virus itself.

Members of the Pharmacy Trials Team
“In an average month, the pharmacy team would normally get involved in around four new different clinical trials; reviewing and approving the medication, and working with the research and development team to ensure that staff are well supported and the drugs can be delivered safely to our patients.
“Because coronavirus was taking such a strong hold so quickly, there was a huge drive to discover ways of reducing the severity of the virus, lessening the duration of patients’ illness, and finding a vaccine.
“In one month alone, we almost doubled that figure with seven new clinical trials, all centred on COVID-19, starting within the Trust. The most widely known trial we took part in was an international study for Remdesivir, for which we recruited around 20 patients. This trial has now concluded and the collated evidence does indeed suggest that appropriate use of this drug can lessen the time for which a patient is ill with coronavirus, so this was something really worthwhile to have been involved in and something we know will make a difference going forward. We’d really like to thank those patients who took part the trial locally and contributed to our learning.
“The latest trial to begin locally is that for a coronavirus vaccine. Working with colleagues in infectious diseases and research and development, both locally and Oxford-based, the team has screened more than 350 members of NHS staff for the trial which is now underway.
“Working on trials has seen pharmacy staff working late into the evenings to ensure that patients involved in complex trials, who might need their medication at night, could still access this safely.”
Paul says pharmacy staff have also stepped into the breach left by doctors redeployed to the COVID front line:

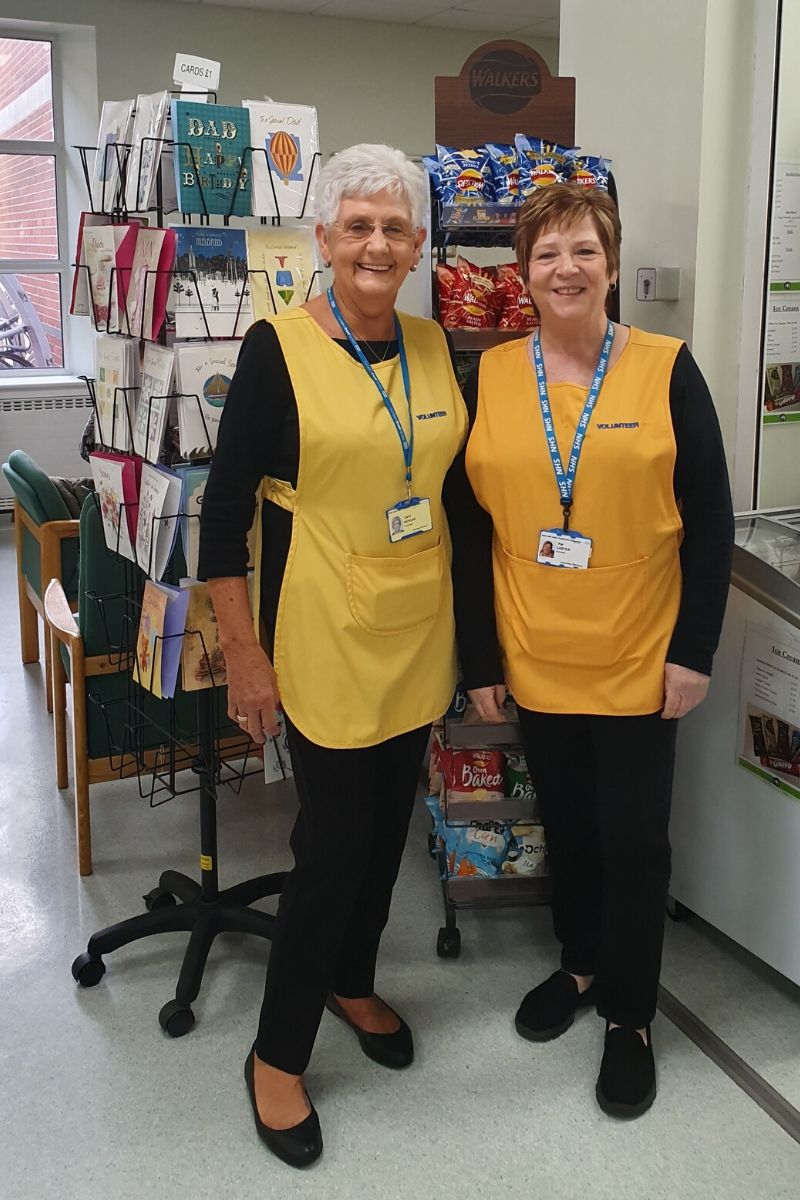
Members of the Clinical Pharmacy Team
“Thousands of hospital appointments were being cancelled during March, April and May, and as many as 20 per cent of our medics were redeployed from their existing roles to support the COVID effort.
“Pharmacists and our pharmacy technicians, who were fast learning and quick to adapt to working in different ways, were able to step up and help to support patients, such as those being treated for cancer, by ensuring their medications could still be prescribed safely and without interruption.
“The focus for many people and indeed for our hospitals became very much COVID-19, but of course the demand for drugs and for medications advice for other conditions didn’t go away. Emergency surgery was still going ahead, patients on our wards still needed pain relief, and treatments for cardiac issues, stroke and cancer didn’t stop. Patients were still being discharged from hospital, either to continue their recovery at home or for end-of-life care, and in the latter case we worked closely with our colleagues in community pharmacy and GP practices, to ensure people could die with dignity, and as symptom free as possible, in their own homes.
“Pharmacy staff, including those working on our aseptic unit, made sure that what would be considered our day-to-day work of preparing chemotherapy doses, making up nutritional packs for patients who can’t eat, preparing patients’ discharge medication and keeping our wards and departments supplied and supported, still went ahead.
“Pharmacy may not be the first team of health workers that people think of when it comes to coronavirus, but their round-the-clock input, both behind the scenes and on the front line, has been invaluable throughout our hospitals. They’ve helped to treat our COVID patients, helped to innovate, and helped to keep the routine work going at an unprecedented time; I’m really proud of the team and hugely grateful for all their support.”



















 With so much of our hospitals taken up with COVID-19, we’re also working with the independent hospital sector to send some of our patients there for appointments and procedures. So, your appointment letter may ask you to attend the Spire Hospital in Anlaby.
With so much of our hospitals taken up with COVID-19, we’re also working with the independent hospital sector to send some of our patients there for appointments and procedures. So, your appointment letter may ask you to attend the Spire Hospital in Anlaby. We have to make sure we’ve got enough PPE to keep our staff and patients safe. The supply issues caused by the global demand are well-known. We will not reintroduce a service unless we have the PPE to keep our teams and our patients as safe as possible.
We have to make sure we’ve got enough PPE to keep our staff and patients safe. The supply issues caused by the global demand are well-known. We will not reintroduce a service unless we have the PPE to keep our teams and our patients as safe as possible.