What is National AHPs (#AHPs) Day?
AHPs Day is a social movement to allow us to come together and focus on our professions. It is a chance to recognise the contribution of Allied Health Professionals, and a chance to celebrate our skills and achievements with colleagues and the public. Our 14 professions make up the 3rd largest workforce in the NHS, but can you name all of the professions and describe their roles?
 Who are Allied Health Professionals?
Who are Allied Health Professionals?
Art Therapists, Drama Therapists, Music Therapists, Chiropodists and Podiatrists, Dietitians, Occupational Therapists, Operating Department Practitioners, Orthopists, Osteopaths, Paramedics, Physiotherapists, Prosthetists and Orthotists, Radiographers, and last but by no means least Speech and Language Therapists.
All qualified Allied Health Professionals are statutorily regulated by the Health and Care Professions Council. The professions have protected titles and are governed by an ethical code, to ensure that they always work to the highest standard.
Who are the Allied Health Professionals who work at Hull University Teaching Hospitals NHS Trust?
Dietitians:
Registered dietitians assess, diagnose and treat diet and nutrition problems at an individual and wider public health level. Dietitians translate the most up-to-date public health and scientific research on food, health and disease into practical guidance to enable people to make appropriate lifestyle and food choices. Their advice influences food and health policy across the spectrum from government to local communities and individuals.
Occupational Therapists:
Occupational therapists provide practical support to empower people to facilitate recovery and overcome barriers preventing them from doing the activities (or occupations) that matter to them. This support increases people’s independence and satisfaction in all aspects of life. “Occupation” as a term refers to practical and purposeful activities that allow people to live independently and have a sense of identity. This could be essential day-to-day tasks such as self-care, work or leisure.
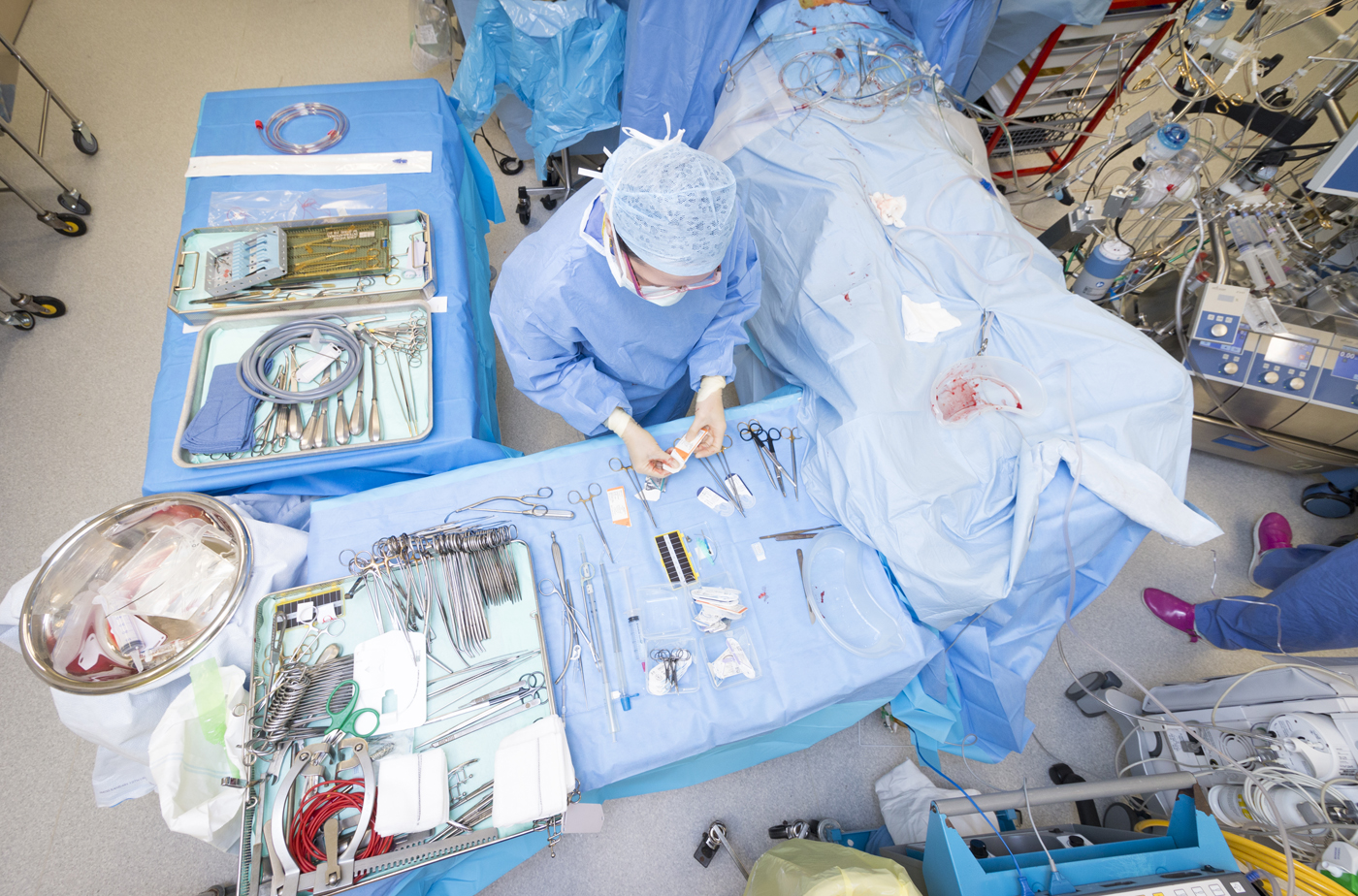
Operating Department Practitioners:
Operating Department Practitioners support patients before, during and after surgery. This includes assessing them after surgery to make sure that they can be taken back to the ward. Their daily duties could include preparing the operating theatre and equipment; making sure specialist equipment is available for specific procedures; monitoring theatre cleanliness; ordering and rotating items of stock and drugs; providing the surgical team with the items they need during an operation; monitoring instruments; and keeping accurate records.
Orthopists:
An orthoptist assesses, diagnoses, treats and monitors a variety of eye disorders. They have expertise in how the eyes move and work together. Orthoptists specialise in the assessment of visual function, particularly in children and those with communication difficulties, and understand why and how neurological defects affect how we see. They assess, diagnose, treat and monitor visual impairment associated with long term conditions including multiple sclerosis, glaucoma, cardiovascular disease, special educational needs and learning disabilities. They can also identify signs which indicate life threatening conditions such as discreet or subtle eye movement disorders in brain tumours, diabetes and those at risk of stroke.
Orthoptists treat double vision, give eye exercises and compensatory strategies and advice in patients recovering from traumatic brain injury ocular trauma, stroke or those who have fallen.
Paramedics:
Most paramedics work for NHS ambulance services. They deal with a range of situations, from minor wounds and substance misuse to serious injuries from fires and major road, rail and industrial accidents. Their daily tasks could include:
- checking a patient’s condition to decide what action to take
- using electric shock equipment (a defibrillator) to resuscitate patients
- carrying out surgical procedures like inserting a breathing tube
- giving medicines and injections
- dressing wounds and applying supports for broken bones
- delivering babies
- working closely with the police and fire services
- keeping accurate records and checking equipment
Physiotherapists:
Physiotherapists help restore movement and function when someone is affected by injury, illness or disability through movement and exercise, manual therapy, education and advice. They maintain health for people of all ages, helping patients to manage pain and prevent disease.
 Podiatrists
Podiatrists
Assess, diagnose and treat conditions affecting the feet and associated structures. Podiatrists can specialise in sports and musculoskeletal foot conditions, diabetic foot management, childrens conditions, homeopathy, dermatology, forensics and education.
Prosthetists and Orthotists:
A prosthesis is a device that replaces a missing body part. Prosthetists design and fit artificial limbs (prostheses) to replace those lost through amputation or limbs missing at birth.
An orthosis is fitted to an existing body part. Orthotists design and fit surgical appliances (orthoses), such as braces, callipers, neck collars and splints. These can be used to support limbs or the spine to relieve pain, aid movement or prevent physical conditions getting worse.
They may work alongside other healthcare professionals such as physiotherapists, who would oversee the patient’s exercise regime; and occupational therapists who would train the patient in how to perform daily activities with the device.
Radiographers:
Radiographers take images of the insides of patients’ bodies to diagnose injury or disease. They also care for and treat people with cancer.
Diagnostic radiographers work in areas that include X-ray, Ultrasound, Fluoroscopy, Computerised Tomography (CT), Magnetic Resonance Imaging (MRI), Nuclear Medicine, Angiography and Mammography.
Therapeutic radiographers are responsible for the planning and delivery of accurate radiotherapy treatments using a wide range of technical equipment. Accuracy is critical, for example, the aim of treatment may be to treat a tumour and destroy diseased tissue while minimising the amount of radiation exposure to surrounding healthy tissue.
Together both diagnostic and therapeutic radiography professionals provide essential services every year to millions of people.
Speech and Language Therapists.
Speech and language therapy provides treatment, support and care for children and adults who have difficulties with communication, or with eating, drinking and swallowing.
Speech and language therapists work with parents, carers and other professionals, such as teachers, nurses, occupational therapists and doctors.




 Who are Allied Health Professionals?
Who are Allied Health Professionals?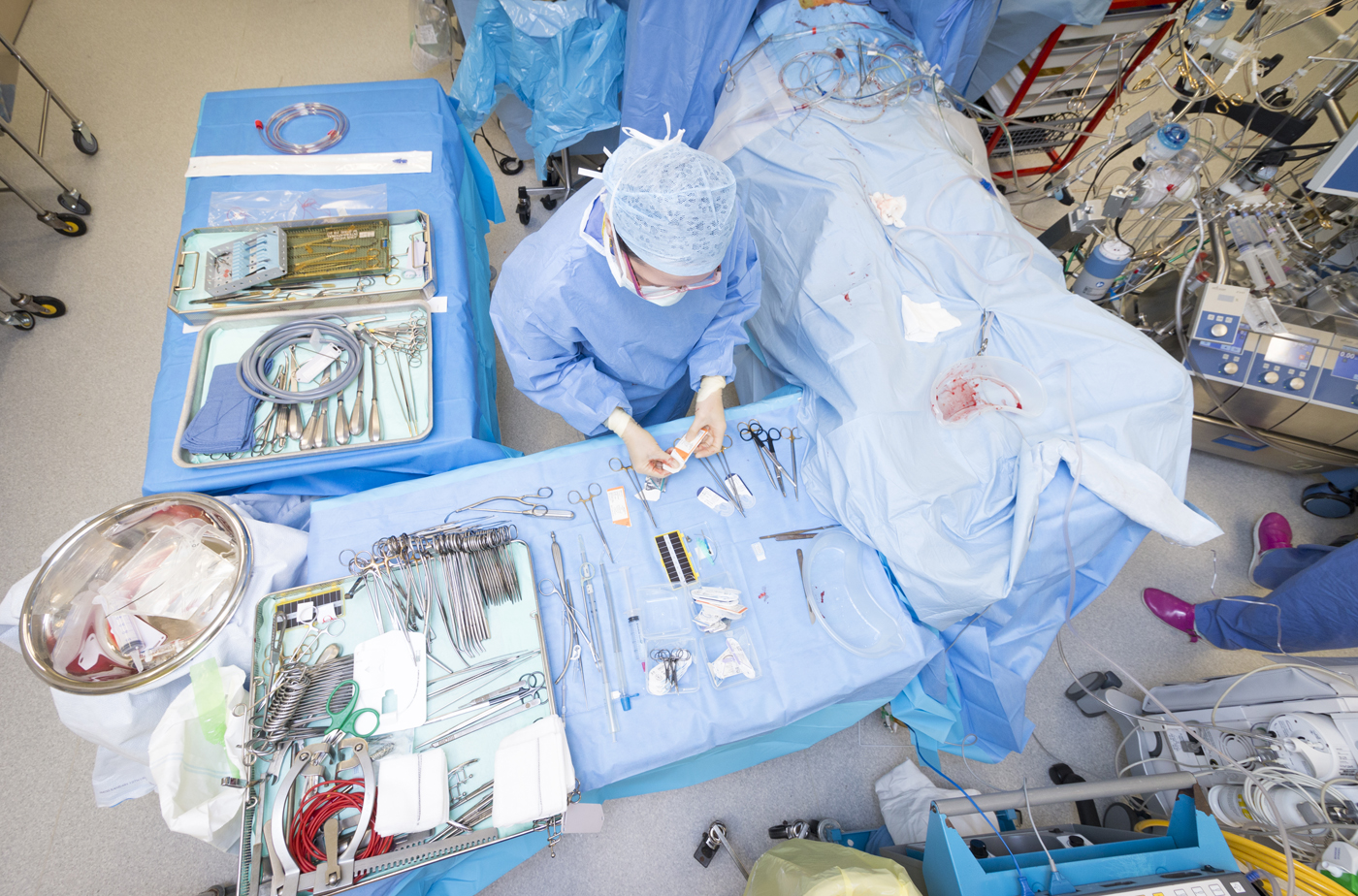
 Podiatrists
Podiatrists





 SIDS claims the lives of around 240 babies in the UK, with five dying every week.
SIDS claims the lives of around 240 babies in the UK, with five dying every week.


