WISHH, the official charity of Hull Hospitals has launched its annual appeal, ‘Space to Grow’ to raise £100,000 to enhance the facilities of Hull’s NICU.
This will complement the Hospital Trust’s expansion of the unit by 5 cots. Each year, Hull Hospitals’ Neonatal Intensive Care Unit (NICU) cares for over 500 premature babies, some stay for hours or days, whilst others stay for weeks and months.

Francesca Mathews (L) Tracey Omar (M) and Jack Jowitt
Hull is one of four Level 3 NICU’s within the Yorkshire and Humber region, caring for babies from 22 weeks gestation offering specialist intensive care for babies locally and across the country. Through the appeal, funds raised will enable WISHH to create:
« A sensory room to enable babies to learn and develop new connections in their brain through light and sound stimulation.
« Development of siblings’ facilities – to enable siblings to play whilst families visit, helping to alleviate the stress parents are already going through.
« Enhancement of the current parents’ facilities – to create a parents ‘Haven’ to allow them to discuss sensitive issues in a calming environment, whilst also allowing them space to gather their thoughts.
« Creation of a staff training facility – to create a fresh and contemporary learning environment for neonatal staff.
Francesca Matthews, Neonatal Ward Manger said, “Due to the complexity of medical needs, more babies are staying for up to 49 gestational weeks. These ‘older’ babies and their families would greatly benefit from sensory stimulation to support their developmental process, ensuring excellent clinical care alongside vital developmental support. Such facilities will also provide these families with a degree of normality, being able to interact within a calming and creative environment with their baby.
“Parents and families who are spending time on the unit for extended periods, will greatly benefit from the new sibling’s and parent’s facilities enhancing and improving their experience at what is a very difficult time. Training is also paramount for our staff and to have a dedicated space will enable educators to deliver specialist training to team members.”
The ‘Space to Grow’ appeal launch has received a fantastic start of £26,000 towards the appeal’s fundraising goal, donated by inspirational fundraisers who all have their own stories to tell on how Hull NICU has touched their lives. These include schoolboy Jack Jowett aged 8, inspired by following in the footsteps of his friend Riley whose baby cousins were cared for by the unit.
Further funds have been raised by members of Beverley Cricket Club, after their Skipper’s wife and baby received lifesaving care from the unit and hospital. Victoria Beadle, championed NICU to her work colleagues and the team at Siemens Gamesa, who adopted WISHH and the Neonatal Unit as their Charity of the Year for 2022, following the care of her twins.
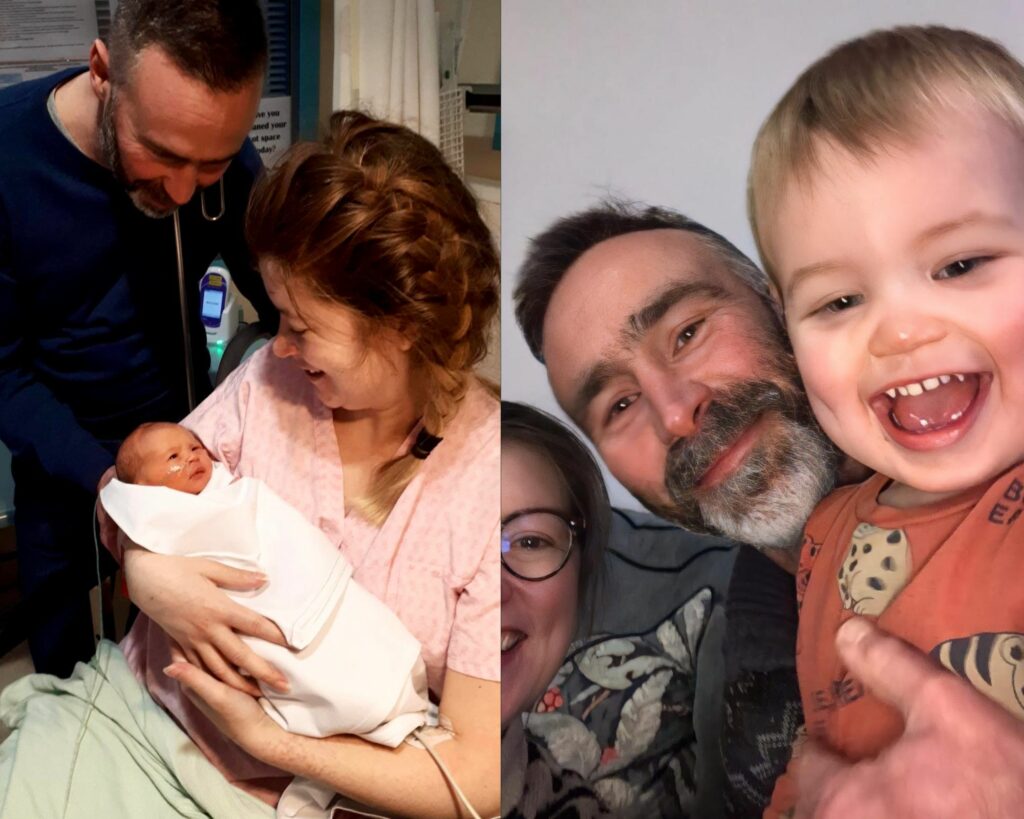
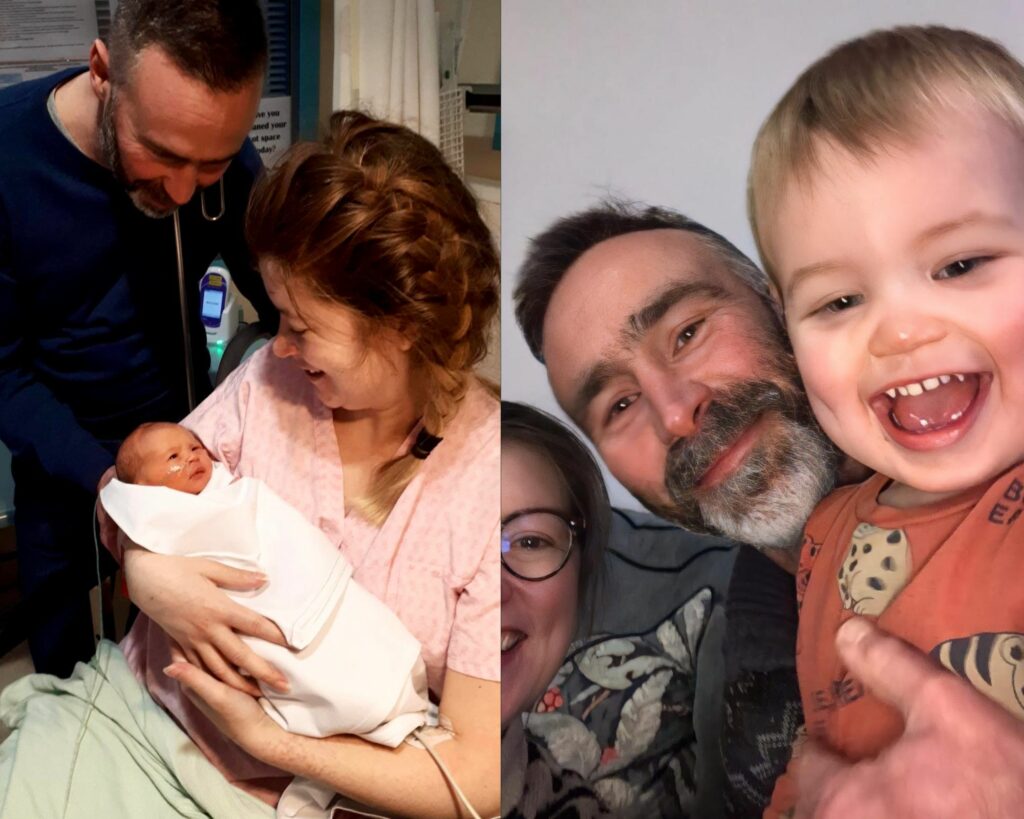
Kevin, Lottie and Gabriel then (L) and now (R)
Sue Lockwood, Chair of the WISHH Charity said, “When Neonatal staff in Hull set out their plans to make improvements to benefit premature babies and their families and asked WISHH for our help, trustees had no hesitation giving our support. We are delighted to launch the WISHH Charity’s ‘Space to Grow’ Appeal to raise £100,000. The improvements needed are over and above what can be provided by the NHS.

Sue Lockwood
“Parents who have had their pre-term baby cared for in Neonatal Intensive Care know that alongside the highly complex clinical skills needed for their tiny babies, the impact and strain on the family is significant. Many difficult days and nights are spent alongside their infant and family engagement is so important. Current facilities don’t always make that easy. Please help us reach our target in any way you can.”
WISHH are inviting members of our community, schools and local businesses to get in touch to become involved by pledging support of our ‘Space to Grow’ appeal.’ To become involved or for further information, contact Lisa Whitton, WISHH Charity Manager lisa.whitton3@nhs.net or call on 01482 622299.
Donations can be made via our Just Giving Page rebrand.ly/SpaceToGrowDonate WISHH have opportunities through places at events to support the appeal, from the Hull Half Marathon on the 11th June, NHS Big Tea, 5th July, The Yorkshire Three Peaks on 9th September. Supporters can choose their own creative way to support our appeal. Businesses are welcome to get in touch to find out how to become an integral part of the appeal.
Supporters can post a cheque made payable to “WISHH Charity” – writing on the reverse ‘Space to Grow Appeal’, posting it to us at WISHH Charity Space to Grow Appeal, First Floor Administration Block, Castle Hill Hospital, Castle Road, Cottingham, HU16 5JQ.
Quotes from fundraisers who have pledged their support:
Jack Jowitt, Aged 8, Beverley

Jack’s hair length
Jack’s close friend Riley, witnessed first-hand the love and care his baby cousins received from staff at Hull NICU and wanted to raise funds to support the work of the unit. Sadly, Riley lost his life at the age of 15 and Jack was determined to follow in his friend’s footsteps to continue his fundraising, having his long hair cut to support NICU.
Jack, through the help of family and friends raised over £9,000. When we asked why he was cutting his hair, Jack answered, “I’m doing it for charity and for Riley, to fulfil his wishes”.
Beverley Cricket Club
The club’s third team skipper Kevin and his wife Lottie were looking forward to the birth or their baby, when unexpectedly they both needed urgent lifesaving care. Thanks to the brilliance of the excellent NHS staff, their son, Gabriel, was successfully delivered and cared for in the Neonatal Intensive Care Unit, Lottie’s life was also saved. In recognition of the wonderful care they both received, the club took part in the Lyke Wake Walk, involving 62 participants aged from 12 to 64 years, who came together and walked over 40 miles in a day raising over £9,700!
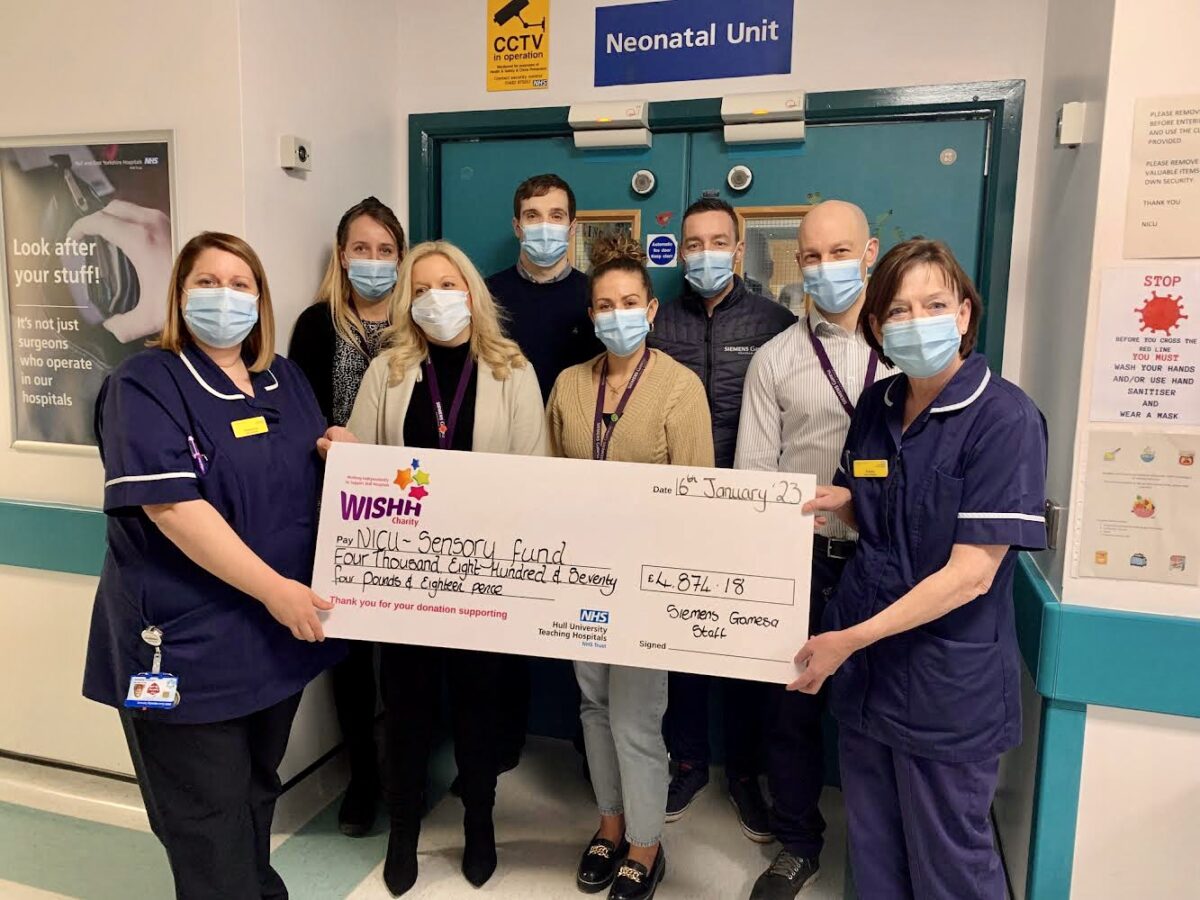
Siemens Gamesa, Hull
Victoria Beadle, of Siemens Gamesa and founder of The Fabulous Fletcher Fund in memory of her son. Victoria and her family are heavily involved in supporting NICU, funding a ventilator, two photo therapy lamps and provided thousands of smaller items to support families staying in NICU, including children’s books, knitted items, blankets, incubator covers, baby nests and care packages for parents who arrive with no personal belongings due to emergency situations. Victoria rallied the support of colleagues across Siemens to vote for NICU/WISHH as their chosen charity of the year with staff taking part in the Hull 10k and holding other fundraising events raising over £4,800.
Photos for illustration purposes and interviews availabile upon request by contacting Lisa Whitton 01482 622299.
Photos to illustrate the appeal and of supporters attached. Provided with consent from the WISHH Charity.
About WISHH
The WISHH Charity is an independent charity created in 2016 supporting Hull Hospitals. The Charity raises funds through appeals and donations to improve and enhance facilities, equipment and services at Hull Royal infirmary and Castle Hill Hospital for the benefit of patients, visitors and staff. For more information, visit our website www.wishhcharity.org.uk or follow us across social media @WISHHcharity
About Hull Hospitals
Hull University Teaching Hospitals NHS Trust has approximately 1,000 inpatient beds, employs more than 10,000 full and part-time staff and provides planned and emergency hospital services for almost 603,000 people in Hull and the East Riding.
It also provides specialist and tertiary services to a 1.25m population from North Yorkshire to North Lincolnshire.
Hull Royal Infirmary provides acute medical and surgical services as well as emergency care. Castle Hill Hospital is the main site for cardiac and planned surgical services and is the regional centre for oncology and haematology.
A Major Trauma Centre for the region, the Trust provides critical care services, with beds for intensive care and high dependency at both Hull Royal Infirmary and Castle Hill Hospital. It also runs the Eye Hospital and Hull Women and Children’s Hospital, which includes a 26-cot neonatal intensive care unit and four transitional care beds.








 Results from HUTH’s annual staff travel survey show the number of staff driving to Hull Royal Infirmary and Castle Hill Hospital in Cottingham has declined significantly, with corresponding increases in staff switching to public transport, cycling or walking to work.
Results from HUTH’s annual staff travel survey show the number of staff driving to Hull Royal Infirmary and Castle Hill Hospital in Cottingham has declined significantly, with corresponding increases in staff switching to public transport, cycling or walking to work.
 The trust worked with bus firms East Yorkshire Buses and Stagecoach so staff could board three new bus services for free anywhere along the routes, just by showing their ID badges. Figures show 10,000 journeys were made on these new services in the first nine months of the scheme.
The trust worked with bus firms East Yorkshire Buses and Stagecoach so staff could board three new bus services for free anywhere along the routes, just by showing their ID badges. Figures show 10,000 journeys were made on these new services in the first nine months of the scheme.

 Chris Long, Chief Executive at HUTH, performed the official opening of the trail by unveiling a plaque to thank the gardeners for their work in clearing a trail through the woods.
Chris Long, Chief Executive at HUTH, performed the official opening of the trail by unveiling a plaque to thank the gardeners for their work in clearing a trail through the woods.