Ambulance service colleagues have announced that industrial action by both GMB and Unison members will be taking place on Wednesday 11 January 2023.
In readiness, we have been working to discharge as many patients as possible from hospital in advance of the strike, where those patients are medically fit and it is safe to do so.
Anyone with a hospital appointment on 11 January should continue to attend as normal unless contacted to advise otherwise. Should any changes become necessary as we approach the strike date, for example if an appointment has to be rescheduled or patient transport arrangements need to be changed, affected patients will be contacted directly to discuss in more detail.
Members of the public should be aware that there will be fewer ambulances on the roads during industrial action and they will be prioritising the most urgent and life-threatening calls. As a result, we will be stepping up efforts on the day to support timely ambulance turnaround for those crews arriving at our Emergency Department.
There are also likely to be fewer 999 and NHS111 call handlers available on the day and anyone contacting these services should expect longer call response times.
Anyone with non-urgent care needs should first seek help from NHS 111 online.
If you are unwell and need assistance, you should also consider alternatives such as:
- Local pharmacies
- Your GP practice
- Story Street walk-in centre, Hull
- Local Urgent Treatment Centres (Bransholme, Beverley, Goole and Bridlington), all of which are open into the evening with the exception of Bransholme which remains open 24hrs/day.
Regardless of any strike action taking place, it is really important that patients who need urgent medical care continue to come forward, especially in emergency and life-threatening cases – when someone is seriously ill or injured, or their life is at risk.









 Hull University Teaching Hospitals (HUTH) has teamed up with phone charging company Joos to provide power banks in its Children’s A&E and its Emergency Care Area (ECA) at Hull Royal Infirmary.
Hull University Teaching Hospitals (HUTH) has teamed up with phone charging company Joos to provide power banks in its Children’s A&E and its Emergency Care Area (ECA) at Hull Royal Infirmary.
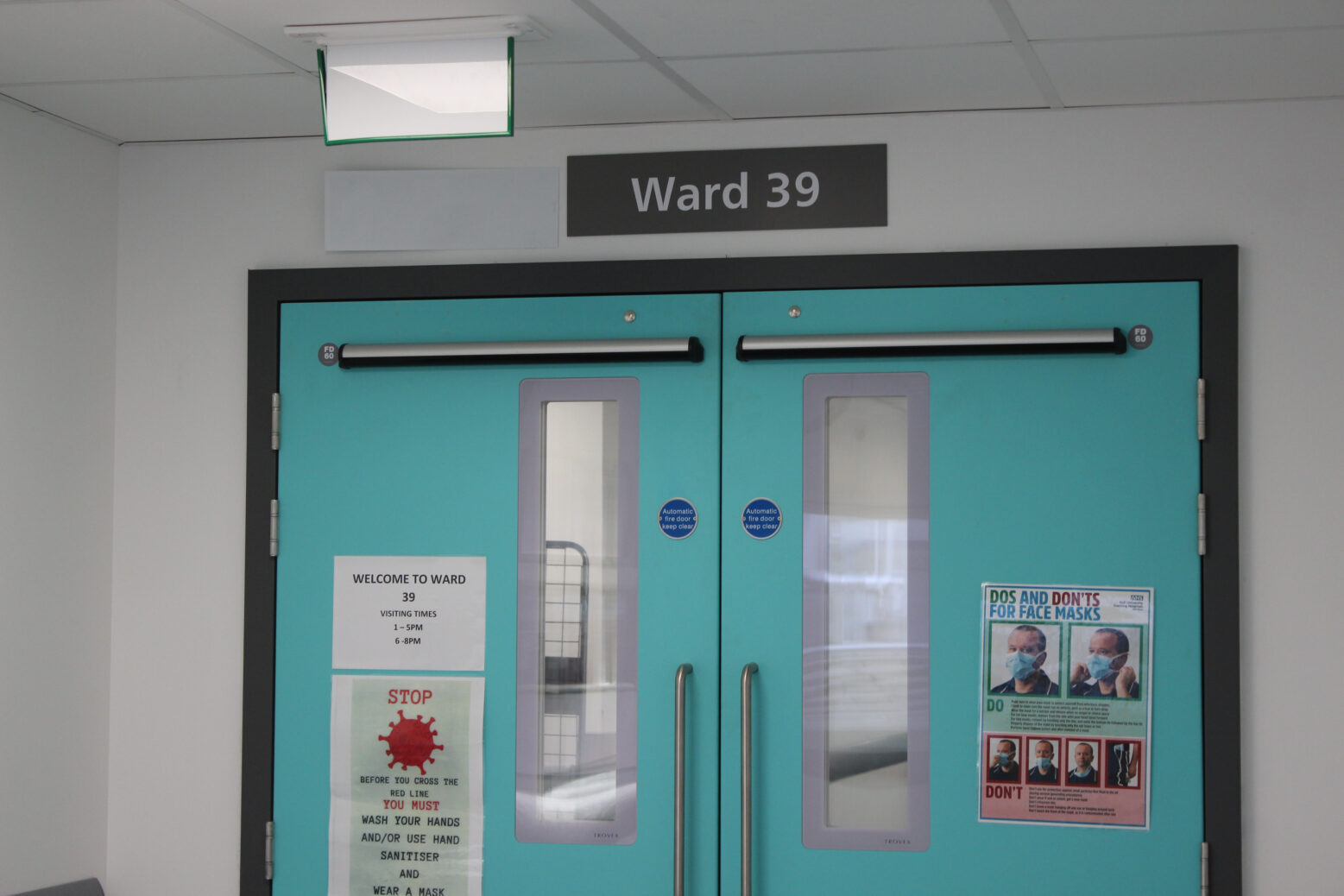
 “However, those who require assessment or stabilizing will now go to our new ward under the care of specialist cardiology nurses and cardiologists instead of being transferred by ambulance across the city to Castle Hill.
“However, those who require assessment or stabilizing will now go to our new ward under the care of specialist cardiology nurses and cardiologists instead of being transferred by ambulance across the city to Castle Hill.

 Around 90 per cent of student nurses at the University of Hull now come to work at Hull Royal Infirmary and Castle Hill Hospital since the launch of the campaign five years ago.
Around 90 per cent of student nurses at the University of Hull now come to work at Hull Royal Infirmary and Castle Hill Hospital since the launch of the campaign five years ago.