At NHS Humber Health Partnership we’re proud to say that we employ hugely talented people from across the globe – 112 different nationalities to be precise!
And, while we value and appreciate every single person, no matter where they hail from, as today is NHS Overseas Workers Day we wanted to take the opportunity to celebrate the achievements of all those who have travelled to our area to help care for you.
They bring a wealth of skills and experience in everything from clinical care to developing others – and we don’t know where we’d be without them.
We hope you’ll join us in thanking every single member of staff for their ongoing dedication and commitment in helping to make our communities better.
Their stories

Valerie, our head of Occupational Development, Inclusion and Wellbeing is originally from Lyon, France, but first came to the Humber region in the 1990s, studying in Hull.
It’s fair to say that she has a real passion for learning and inclusion – both in work and in her personal life – enjoying spending her free time studying foreign languages, spirituality, philosophy, and religion, when she’s not tending her fully-organic allotment or spending time with her family that is!
That love of learning and helping others to develop has also helped to shape her career.
She said: “I moved to the UK in 1998 and after working a few years in the export and import sector and international logistics, I realised I was enjoying training and development a lot.
“At the same time, I developed a fascination for tech and the boom of the internet offered me opportunities in online education and instructional design.”
Her career took her into leading on e-learning for Centrica, moving onto project management for HT and programme management for leadership development; before taking on senior Learning and Development and coaching roles in the wealth management and banking sector in Canary Wharf, London.
Valerie added: “I then moved to Lincoln and after taking a career break to raise my twins, I worked for local government services, before joining the NHS in 2021 as an OD business partner.
“I initially started working for NLaG in 2023 as Head of OD Inclusion and Wellbeing and grow a team of professionals to support culture transformation in the Trust and provide support to staff so that we build an environment where they thrive. What a great opportunity to make your mark isn’t it? I continue to strive to bring that change to the partnership since it was formed a year ago.
“People are our number one asset. I like the diversity of the people who work in the NHS best. I feel that the entire world is represented in all professions here and I see this as a great competitive advantage, to harness the richness of talent, ideas and innovation that people from all cultures and all backgrounds bring to the Partnership.”

It’s hugely important to us that we help our teams to grow and develop – taking on new challenges and achieving their career goals.
So, despite being very sad to see him leave us, we’re immensely proud that working for NHS Humber Health Partnership has helped talented Registered Nurse Ihsan Ullah take on his dream role in research.
Originally from Pakistan, Ihsan graduated with a nursing degree in 2007 and went on to achieve a PhD in Medical Sociology, joining Northern Lincolnshire and Goole NHS Foundation Trust in January 2024 working in Emergency Care.
He said: “My aspiration has always been to progress in my career as a researcher, and I am fortunate to have been appointed to a research role by the Noclor Research Office in London, which I will be joining soon. However, NLaG will always hold a special place in my professional journey, and I will never forget the experiences and support I have received here. I have greatly appreciated the initial efforts of the Practice and Development team, as well as the support from the team on the Integrated Acute Assessment Unit and Same Day Emergency Care unit.
“What I like the most here is the emphasis on continuous professional development, the strong sense of teamwork, the supportive management, and the recognition of individual contributions. These aspects create a positive and motivating work environment.”

A passion for caring for others runs in the family for Nutritional Support Nurse, Esther Okochi.
Originally from Nigeria, her grandmother, mother and aunt were all nurses.
She said: “Growing up amidst these lovely and caring individuals in the noble profession of nursing attracted me to the career.
“Being a nurse myself for 16 years now, has also taught me to be more kind, empathetic and to be more diligent, and has afforded me the opportunity to meet a host of beautiful people from different walks of life. It has also opened me to a plethora of opportunities that I am forever grateful for.”
Esther graduated with a Bachelor of Nursing Science degree and qualified as a Registered Nurse in 2009, before taking on a role as a Nurse Tutor in the school of nursing. From 2011 she moved into clinical roles, working in medical, surgical and orthopaedic wards, along with obstetrics and gynaecology and community nursing.
The busy mum-of-four – who also loves singing, dancing, reading and cooking, as well as creating social media content – took the plunge to move to the UK in 2003, initially working on the Stroke unit.
She said: “I came upon an advert for the Trust and saw that the values aligned with my personal values. Not only that, but I watched the testimonials from other internationally educated staff; Nurses and Doctors. Their shared experiences made me feel at ease, also made me aware that the Trust has its staff well-being at heart. I applied, was fortunate to get a job in the Trust.
“Honestly, I will say I have met some incredible people since working here who have shown me kindness, ready to help to ensure there is professional development and career advancement which for me is vital to attaining job satisfaction, and self-actualization – so I say a big thank you to all the wonderful teams making this happen.”

Although moving to another country and adapting to a different healthcare system has been a challenge, since joining us in 2020 Odunola has soared.
She said: “NHS Humber Health Partnership stood out to me because of its reputation for supporting international healthcare workers and the opportunities available for training and career progression.
“I came here in October 2020 as a dedicated International Professional, with a passion for using my expertise and dedicating myself to patient care. I have worked in Ward 22, the Endoscopy Unit and I am now part of the Occupational Health Department.
“I have been a qualified Professional Nurse Advocate since two years ago and I am proud to be a source of encouragement and support to patients and colleagues.
“Beyond my professional role I have integrated into the local community, building meaningful and lasting relationships.
“What I like best about working here is the warm and inclusive culture, genuine care for staff wellbeing, the commitment to professional development and the diverse and collaborative work environment.”

Originally from Nigeria, Olu was drawn to a career in occupational health nursing because of her “passion for making a real impact in people’s lives—both in their health and their workplace experience.”
She said: “I have always believed that work should be a place where people can thrive, not just survive. The idea of promoting health, preventing illness, and ensuring a safe and supportive working environment deeply resonates with me.
“I love my Job – it is more than just a role; it’s a chance to support people, drive change, and ensure that everyone has the care they need to stay happy, healthy, and productive at work.
And I absolutely love the fact that i have a manager that shares the same vision.
“Beyond work, I’m a proud mum of two energetic boys—a full-time job I absolutely love! I also enjoy cooking because the men in my life sure love to eat.”


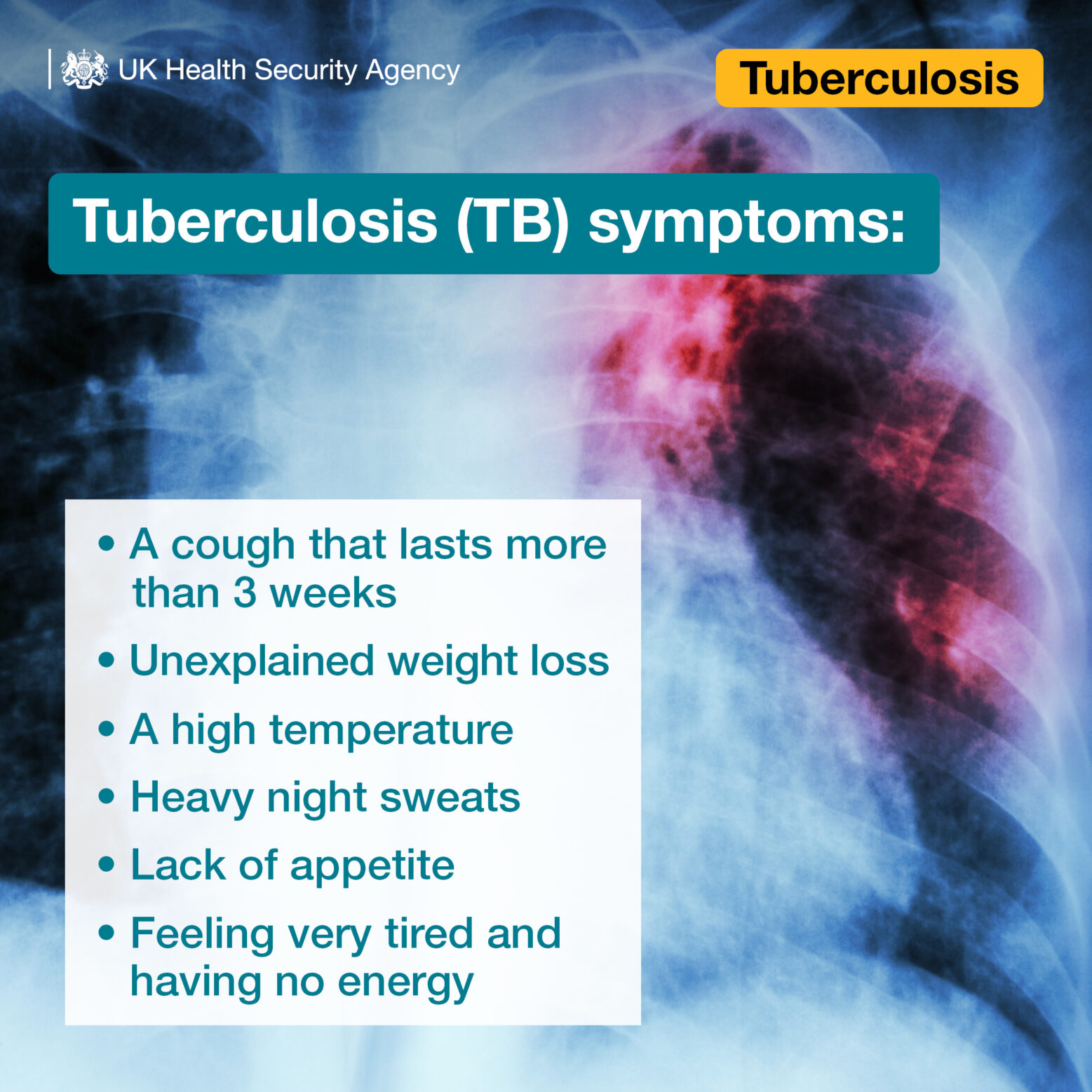
 A specialist in infectious diseases in Hull is warning cases of Tuberculosis (TB) are increasing, with homeless people or those with drug or alcohol addictions at risk.
A specialist in infectious diseases in Hull is warning cases of Tuberculosis (TB) are increasing, with homeless people or those with drug or alcohol addictions at risk.
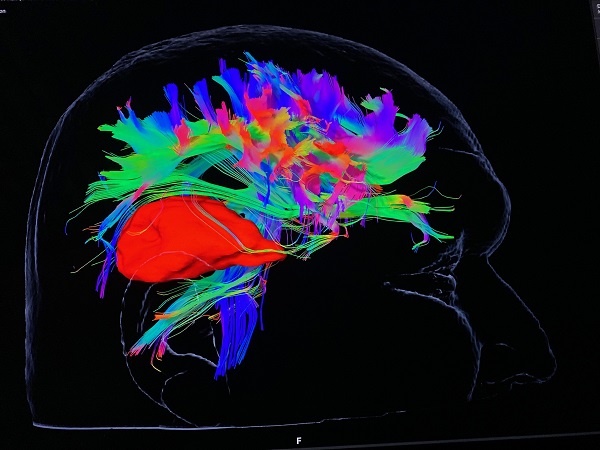
 Consultant Neurosurgeon Chittoor Rajaraman said: “For the first time in Hull, we will be able to use this technology to offer patients safer surgery, with better outcomes.
Consultant Neurosurgeon Chittoor Rajaraman said: “For the first time in Hull, we will be able to use this technology to offer patients safer surgery, with better outcomes.





 He said: “The patients who die with prostate cancer are usually the people who are diagnosed when the disease is at an advanced stage and is then incurable.”
He said: “The patients who die with prostate cancer are usually the people who are diagnosed when the disease is at an advanced stage and is then incurable.”
 It’s a scheme which has helped launch the careers of thousands of young people across Hull and East Yorkshire
It’s a scheme which has helped launch the careers of thousands of young people across Hull and East Yorkshire







