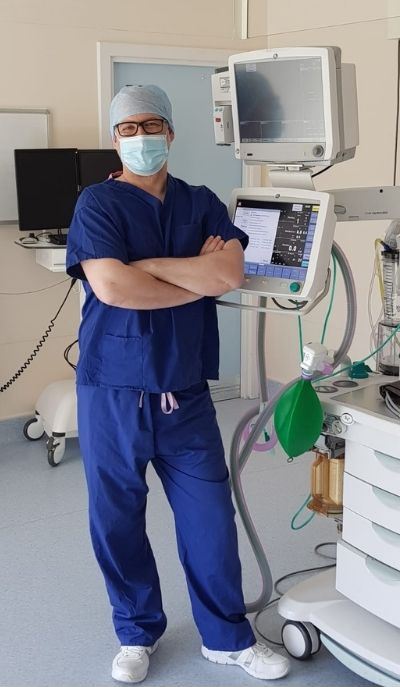
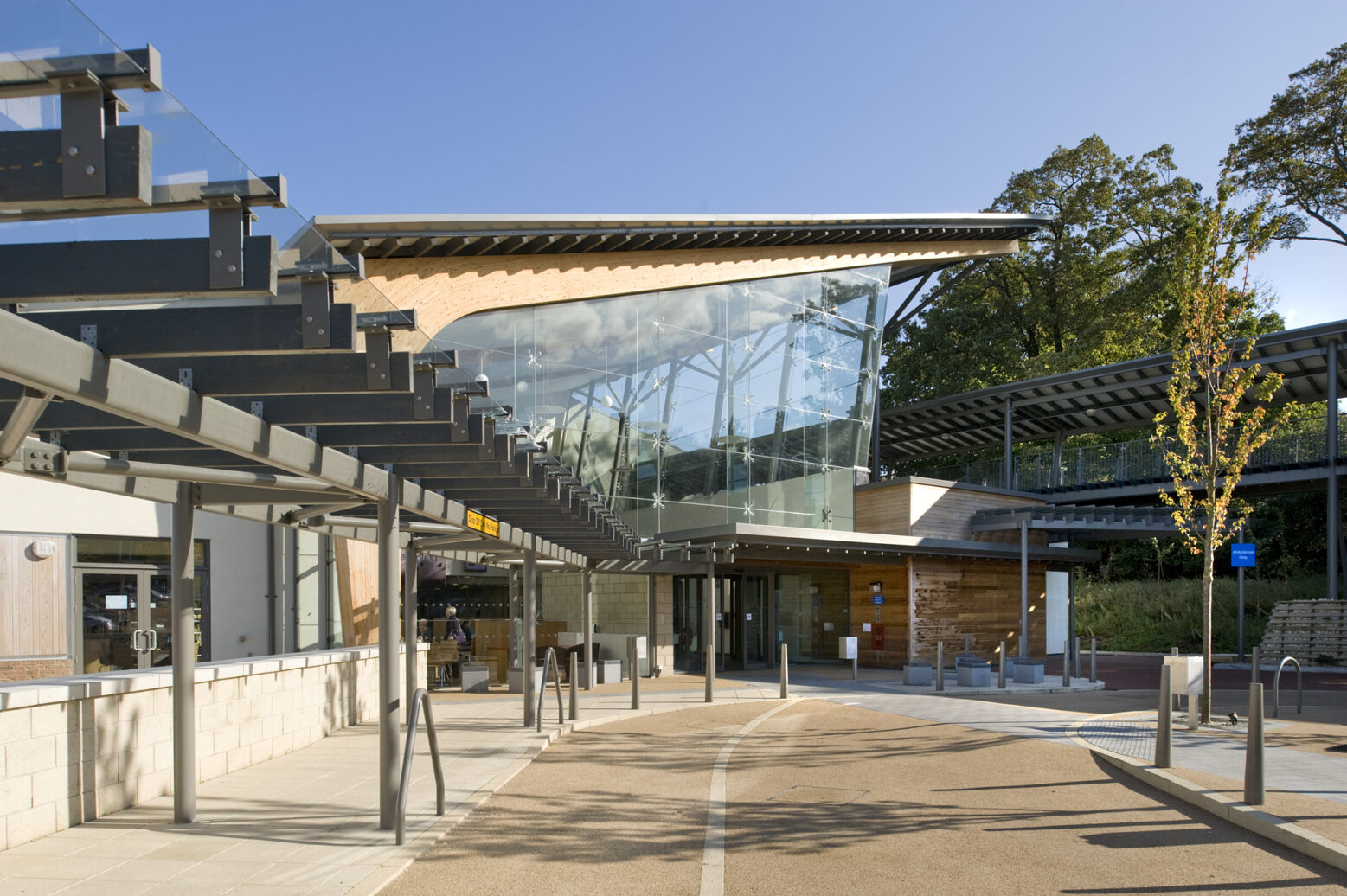
A multi-million pound Intensive Care Unit (ICU) is to open at Hull Royal Infirmary this summer for critically ill and injured patients from all over Yorkshire and Northern Lincolnshire.
Hull University Teaching Hospitals NHS Trust is a Major Trauma Centre for the region and the ICU at Hull Royal Infirmary will provide patients with some of the best critical care facilities in England.
The three-storey building, close to the hospital’s Emergency Department, will also feature modern isolation facilities to “future proof” the trust against a further wave of Covid-19 or another pandemic.
 Chief Executive Chris Long said: “It is testament to the hard work and dedication of our critical care teams that we will be able to take our place at the forefront of critical care in the country and to our Estates team for driving this project in these challenging times.
Chief Executive Chris Long said: “It is testament to the hard work and dedication of our critical care teams that we will be able to take our place at the forefront of critical care in the country and to our Estates team for driving this project in these challenging times.
“This new unit will be a very welcome addition to the outstanding care we can provide people in critical need of emergency treatment, not just here in East Yorkshire but across our wider region.
“It will enable us to save more lives, provide patients and their families with better facilities and ensure we are in the best possible position to deal with any future waves of the virus or, indeed, any other pandemic in the future.”
The foundations for the new 24-bedded ICU were poured in the first week in January with critical care teams expected to move into the new building ahead of the arrival of the first patients in August. The final cost of the unit is expected to be in the region of £8m.
The new ICU is being constructed in line with the trust’s Green Plan and will be as energy efficient as possible with its own heat pumps, air conditioning, chillers and heat recovery systems. This means the unit will remain cool enough for patients and staff in the summer but warm enough in the cooler months.
Patients will undergo life-saving treatment in glass-front cubicles, double the size of the cubicles in the two existing ICUs in the tower block, on the first two floors. Each floor will be split into two identical halves, with a staff observation area in the centre.
 Cubicles will be fitted with negative air extraction systems to assist infection prevention and control, with six cubicles on each floor being fitted with donning and doffing anterooms to enable staff to care for patients with Covid-19 or any other infectious disease.
Cubicles will be fitted with negative air extraction systems to assist infection prevention and control, with six cubicles on each floor being fitted with donning and doffing anterooms to enable staff to care for patients with Covid-19 or any other infectious disease.
Every cubicle will be fitted with a Draegar ceiling pendant for essential services including medical gases to maximize the floor space to allow doctors, nurses and other health professionals to perform their tasks. Electric hoists will also be in place to allow staff to lift patients safely, reducing the risk of musculoskeletal problems in the future.
A dedicated bed lift will connect the ICU to the theatre complex in the main Hull Royal Infirmary tower block via a link bridge over Lansdowne Road. This will also be used to take patients from the ICU for MRIs or scans, preventing the need for them to be wheeled outside to the MRI suite.
A staff-only link staircase will also be created to ensure teams can access the tower block without having to leave the building.
While plans are still awaiting final approval, the top floor of the unit is likely to include two new trauma theatres, with six to eight recovery beds to monitor patients in those critical first few hours after surgery.
As well as increasing theatre capacity at the trust, the new theatre floor will also act as a decant space to allow ongoing maintenance of the existing ICUs throughout the year. The additional space will also enable the trust’s Estates team to begin the work to upgrade the 60-year-old operating theatres in the tower block.
A separate extension is being built next to the ICU to provide support accommodation for staff including rest rooms, offices and support services including Medical Physics.
Duncan Taylor, Director of Estates, Facilities and Development at the trust, said: “This is a fantastic facility which will help us provide the best possible care for our most seriously ill and injured patients well into the future.
“We undertook months of careful planning and design, working hand-in-hand with our clinical colleagues, to design the unit, using our wealth of experience of the pandemic to provide the cutting-edge facilities our teams will need.
“We are confident our new Intensive Care Unit will serve our staff, our services and our patients well for decades to come.”







 Emma Smith, Head of Discharge Liaison Services at the trust, said: “This new system means patients will get the very best care in the most appropriate place for them because they will no longer be kept in hospital once they are well enough to leave.
Emma Smith, Head of Discharge Liaison Services at the trust, said: “This new system means patients will get the very best care in the most appropriate place for them because they will no longer be kept in hospital once they are well enough to leave. New guidance and funding has been introduced by the Government to speed up the process and remove some of the barriers involved in discharging patients efficiently from hospital.
New guidance and funding has been introduced by the Government to speed up the process and remove some of the barriers involved in discharging patients efficiently from hospital.

 Ward Sister Hayley Butler said her entire team, including nursing staff, housekeeper and hygienist, ward clerks, cleaning staff and caterers as well as members of the multi-disciplinary team looking after patients, stepped up to the challenge.
Ward Sister Hayley Butler said her entire team, including nursing staff, housekeeper and hygienist, ward clerks, cleaning staff and caterers as well as members of the multi-disciplinary team looking after patients, stepped up to the challenge.
 Priyai Parkinson, Research Delivery Lead at Hull University Teaching Hospitals NHS Trust, said: “We are looking for volunteers to take part in a study to see what happens in the immune system when a second (boost) dose of Covid-19 vaccine is a different type to the first.
Priyai Parkinson, Research Delivery Lead at Hull University Teaching Hospitals NHS Trust, said: “We are looking for volunteers to take part in a study to see what happens in the immune system when a second (boost) dose of Covid-19 vaccine is a different type to the first. Adult volunteers of 50 years and older who have received one dose of either the Pfizer or AstraZeneca vaccine in the last eight to 12 weeks are being invited to take part in this latest trial, led by the Oxford Vaccine Group, part of the University of Oxford.
Adult volunteers of 50 years and older who have received one dose of either the Pfizer or AstraZeneca vaccine in the last eight to 12 weeks are being invited to take part in this latest trial, led by the Oxford Vaccine Group, part of the University of Oxford.

 Women attending scans to check on the growth of their baby throughout their pregnancy will also be able to bring their partner or another adult from today.
Women attending scans to check on the growth of their baby throughout their pregnancy will also be able to bring their partner or another adult from today.
