There are concerns that the fear of Covid-19 may be deterring cancer patients from receiving vital treatments and tests.
Julie Watson, Macmillan lead cancer nurse at Hull University Teaching Hospitals NHS Trust says patients who are worried about catching coronavirus when they come in to hospital could be delaying treatment or putting off investigations.
Julie explains:
“As the specialist cancer centre for the Humber region, we’ve been working really hard here at the Queen’s Centre to maintain as many routine services as we can for our patients.

Julie Watson, Macmillan lead cancer nurse
“People with cancer can often have low immune systems, which potentially makes them more vulnerable to infection, so we can completely understand why people may be anxious about coming to hospital right now.
“We’ve been working hard for many months to ensure our departments, wards and treatment rooms are made safe for the people using them, and that we invite people to attend the hospital only where there’s an absolute need for them to do so.
“We now carry out consultations by phone or video conference where it’s safe to do so, which is often more convenient for people in many ways. Where people have to see us, for example for chemotherapy or radiotherapy treatment, or for investigations or tests, we try to stagger people’s appointments, we’ve reduced the seats in our waiting areas, and we keep people away from shared or communal areas as far as we can to reduce the risk of transmission.
“Despite all of these steps, ongoing cleaning and regular reassurances, we are concerned that some patients are letting the fear of the coronavirus get in the way of potentially life-saving treatments or life-changing diagnoses.”
One such area where patient concerns are notable are in Endoscopy, where cameras are used inside the body to help in the detection and diagnosis of conditions such as lung cancer, bowel cancer, pancreatic cancer, and cancers of the mouth and oesophagus.
Lucy Holgate, senior sister in the Endoscopy team at Castle Hill Hospital says:
“Every patient who attends for endoscopy is screened and swabbed before they come to hospital, but we are currently seeing a higher number of patients than normal cancelling or just not turning up on the day, and we know a lot of these concerns are Covid-related.
“We know seeing staff in PPE can be upsetting or even frightening for some people, so add that to a procedure which can often be uncomfortable and may even turn out to confirm a cancer diagnosis, and we can completely understand why people may be worried.
“But it’s important to see the bigger picture. It’s vital that people keep their appointments to avoid any delays in their treatment which could directly affect their own health. If people have any concerns or questions about their safety or what’s involved in their procedure, we’d really encourage them to contact a member of the team and talk these through.”
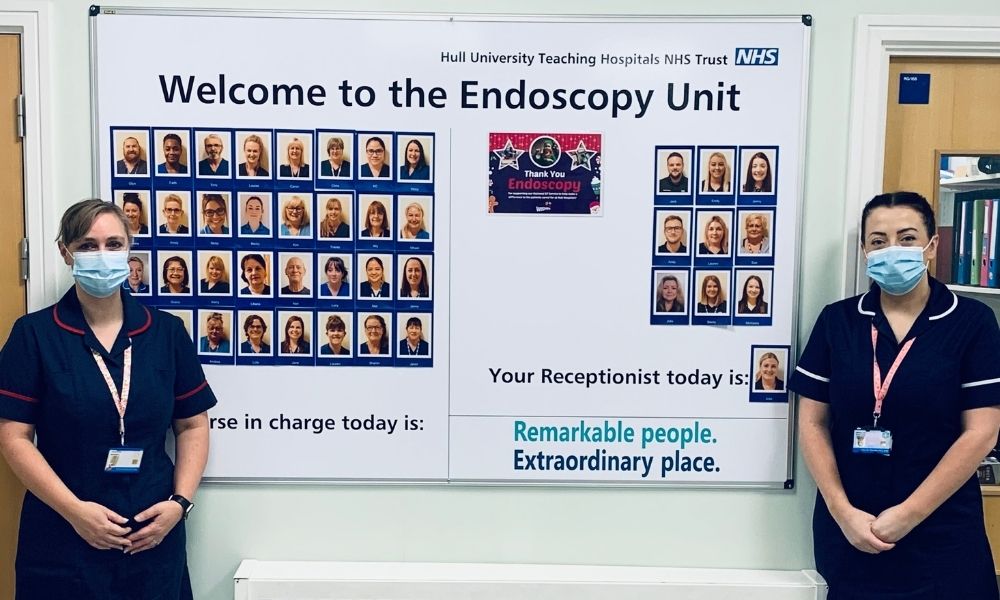
Tracey Davies (left) and Lucy Holgate at the Endoscopy Unit, Castle Hill
As endoscopy is an aerosol generating procedure, staff are required to wear a higher level of PPE than many other departments in the hospital, comprising full face mask, goggles and gown.
“We’ve created special boards, one at Castle Hill and one at Hull Royal to introduce our patients to the team,‘ the face behind the mask’, so people can still get to know us and feel a bit less anxious about their procedure,” says Tracey Davies, lead nurse endoscopist.
The once busy waiting areas and post-procedure recovery area have also been adapted to comply with social distancing rules, to minimise the number of people waiting and the amount of time they spend there.
“The last thing we want is for someone’s health to suffer unnecessarily,” Tracey adds, “so we really would urge people to keep their appointments and to speak to us about any worries they have, as our number one priority is keeping people safe in every way we can.”
The Humber, Coast and Vale Cancer Alliance has worked with the Trust to develop two new videos explaining Covid safety measures to patients in more detail:
Attending appointments during Covid-19 (Castle Hill Hospital)
Accessing cancer services during Covid-19 (Queen’s Centre)
Julie says failure to attend appointments doesn’t just pose a risk to the patient either:
“Non-attendance or late cancellations can also have a knock on effect for the hospital and for other patients. Many of our teams have had to reduce the number of appointments they can safely offer in a day due to enhanced cleaning and infection control processes between patients. Now, due to the need to swab patients before they come to hospital, any appointment which is cancelled at short notice or where the patient simply doesn’t attend can’t be offered to another patient, which means appointment time goes unused and other patients continue to wait who could potentially have been seen sooner.
“Our teams at the Queen’s Centre and Castle Hill are working hard to ensure the safety of all of our patients right now. We know the current situation is worrying, but please help us to help you. If you have symptoms that you are concerned about, please don’t be deterred from seeking help, and if you’re due to undergo tests or receive treatment, you mustn’t let concerns about Covid-19 get in the way of that important, potentially life-saving care.”