Hospital nurses are reshaping a specialist service to keep hundreds of patients most at risk from Covid-19 safe during the pandemic.
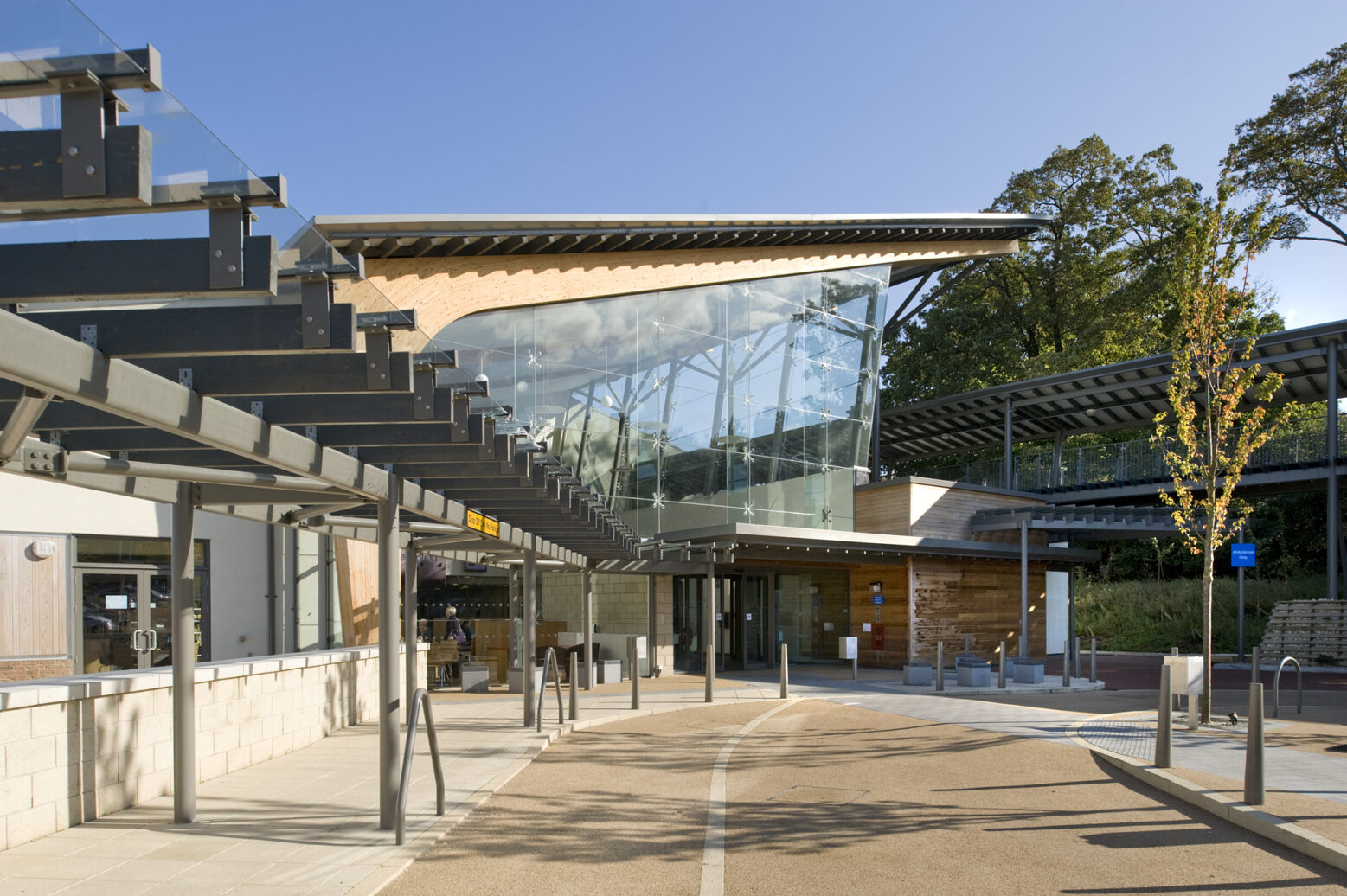
The Home Ventilation team, based at Castle Hill Hospital, supports more than 300 people with severe health conditions affecting their breathing such as Chronic Obstructive Pulmonary Disease, Motor Neuron Disease, Muscular Dystrophy or spinal injuries. People with very high BMIs who experience breathing difficulties are also part of the group.
Every single person helped by the team is classed as “Extremely Clinical Vulnerable” because Covid-19 poses such a danger to their life and most have been shielding for a year to ensure they do not catch the virus.

Our Home Ventilation Team: (from left) Sarah Constable, Halina Voss-Palmer, Diane Murray and Olivia Hardwick
Diane Murray, who leads the team of three nurses, said the service has introduced virtual clinics and socially distanced face-to-face sessions as well as increasing home visits to patients throughout East and North Yorkshire as well as Lincolnshire to keep them safe and as well as possible.
She said: “They are a very vulnerable group of people and dealing with their conditions during Covid-19 has been very challenging.
“Life has got a lot more complicated for us and our patients, most of whom already on ventilators.
“Our workload has changed significantly and we’ve introduced new ways of working to make sure everyone is as safe as possible.”
Virtual clinics have been introduced so patients don’t have to come to hospital as often for check-ups. However, some patients still have to be seen in person to check their readings or their blood gases and collect data from their equipment.
Patients who have to come to Castle Hill Hospital are seen in a socially distanced environments with full infection prevention and control measures in place, with them and staff wearing the appropriate personal protective equipment (PPE) to keep everyone safe.
However, the team still have to carry out home visits for some patients to carry out what is known as “aerosol generating procedures” such as home mechanical ventilation or cough-assist.
These procedures can be dangerous if the patient has the virus because they can produce infected droplets in the air so the team must wear enhanced PPE including special respirator masks, gowns, gloves and visors to keep them safe.
Diane said: “There’s a lot of “doffing and donning” of PPE on people’s doorsteps these days but it’s what we need to do to keep us and our patients safe. This is particularly challenging in the wind and rain. Patients and families need some clear explanations of why we are wearing the level of PPE that they see on the television in ICUs and Covid Wards when we are in their homes.
“They have all been supportive and appear reassured by the measures we are taking to keep them and us safe.
“We’ve received our vaccine now so we’ll have that added layer of protection and our patients have also started receiving the vaccine too because of their clinical vulnerability. We still have to take the precautions with wearing PPE and distance where possible due to the high risk nature of some of the procedures we are performing.
“Sometimes, when we go into the homes of these patients and sit on their sofas, we are the first people they have seen in a very long time because they’ve been shielding at home.”
Diane said patients shouldn’t be worried about coming to hospital for their face-to-face check-ups because of the measures put in place to keep them safe.
“If anyone is worried, I’d ask them to contact the team so we can talk them through the process. It’s really important people keep their appointments and we can always make alternative arrangements for those who aren’t able to come to hospital.
“We also advise our patients to try and wear a mask or face shield if they do have to go out of their homes- they shouldn’t assume because they have a condition that affects their breathing that they cannot wear a mask. Many of our patients are still able to wear masks for short periods and this will help keep them safe.
“Covid-19 is changing how we work and it’s going to be with us for some time yet. The numbers are still higher than the national rate in the areas our patients come from but we are making these changes to keep everyone as safe as possible.”
The Home Ventilation Service can be contacted by calling 01482 624130. You can also email hyp-tr.huth.hmvs@nhs.net to get in touch with the team.



 Emma Smith, Head of Discharge Liaison Services at the trust, said: “This new system means patients will get the very best care in the most appropriate place for them because they will no longer be kept in hospital once they are well enough to leave.
Emma Smith, Head of Discharge Liaison Services at the trust, said: “This new system means patients will get the very best care in the most appropriate place for them because they will no longer be kept in hospital once they are well enough to leave. New guidance and funding has been introduced by the Government to speed up the process and remove some of the barriers involved in discharging patients efficiently from hospital.
New guidance and funding has been introduced by the Government to speed up the process and remove some of the barriers involved in discharging patients efficiently from hospital.

 Ward Sister Hayley Butler said her entire team, including nursing staff, housekeeper and hygienist, ward clerks, cleaning staff and caterers as well as members of the multi-disciplinary team looking after patients, stepped up to the challenge.
Ward Sister Hayley Butler said her entire team, including nursing staff, housekeeper and hygienist, ward clerks, cleaning staff and caterers as well as members of the multi-disciplinary team looking after patients, stepped up to the challenge.
 Priyai Parkinson, Research Delivery Lead at Hull University Teaching Hospitals NHS Trust, said: “We are looking for volunteers to take part in a study to see what happens in the immune system when a second (boost) dose of Covid-19 vaccine is a different type to the first.
Priyai Parkinson, Research Delivery Lead at Hull University Teaching Hospitals NHS Trust, said: “We are looking for volunteers to take part in a study to see what happens in the immune system when a second (boost) dose of Covid-19 vaccine is a different type to the first. Adult volunteers of 50 years and older who have received one dose of either the Pfizer or AstraZeneca vaccine in the last eight to 12 weeks are being invited to take part in this latest trial, led by the Oxford Vaccine Group, part of the University of Oxford.
Adult volunteers of 50 years and older who have received one dose of either the Pfizer or AstraZeneca vaccine in the last eight to 12 weeks are being invited to take part in this latest trial, led by the Oxford Vaccine Group, part of the University of Oxford.

 Women attending scans to check on the growth of their baby throughout their pregnancy will also be able to bring their partner or another adult from today.
Women attending scans to check on the growth of their baby throughout their pregnancy will also be able to bring their partner or another adult from today.

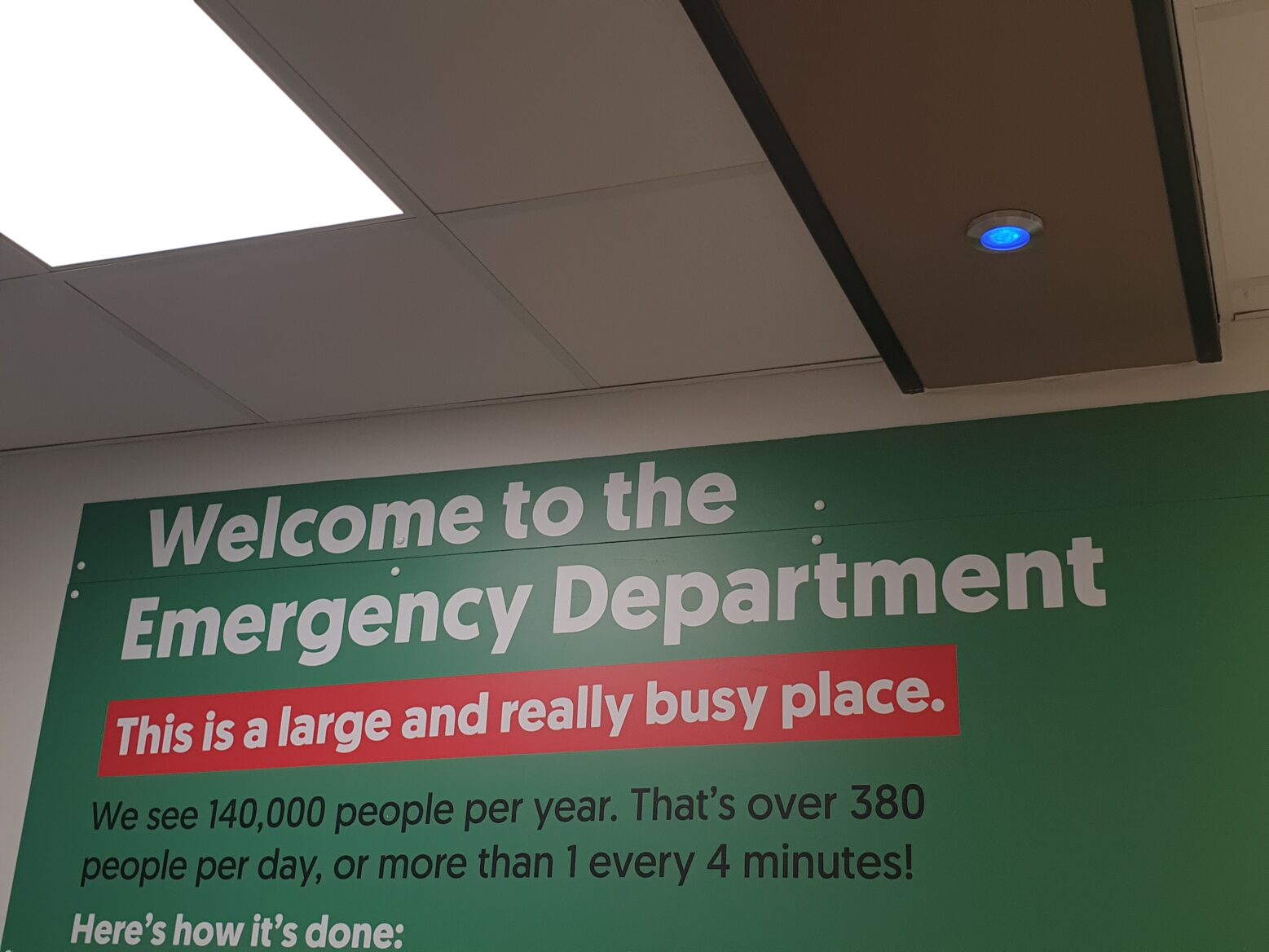

 These changes are possible due to the falling number of cases of Covid-19 in our area along with some extra precautions in place such as extra screens and the use of a remote buzzer system, similar to those used in some restaurants, to allow women and the person with them to maintain safe social distancing whilst waiting in the hospital.
These changes are possible due to the falling number of cases of Covid-19 in our area along with some extra precautions in place such as extra screens and the use of a remote buzzer system, similar to those used in some restaurants, to allow women and the person with them to maintain safe social distancing whilst waiting in the hospital.