More than 20,000 light fittings are to be replaced at Hull’s hospitals as part of an environmental quest to reduce deaths caused by air pollution.
Hull University Teaching Hospitals NHS Trust is working towards a government target to become carbon neutral by 2040.
Now, every light fitting at Hull Royal Infirmary and Castle Hill Hospital as well as the trust’s smaller hospital sites around the city is to be replaced with SMART LED lighting after the trust was awarded a £12.6m grant to support its major green agenda.
Marc Beaumont, Head of Sustainability, said: “This scheme will have a major impact by saving energy and carbon emissions.
“In Hull alone, air pollution causes 128 deaths each year. These are our people – our friends, our neighbours and our loved ones – and we must take steps to do what we can to prevent these unnecessary deaths.
“As well as reducing our emissions, this replacement project will improve lighting levels throughout our buildings, benefitting patients, visitors and staff.”
 As the largest employer in our region, the trust is recognising its duty to look after this part of the world, not just the one million plus patients who come to hospital for treatment.
As the largest employer in our region, the trust is recognising its duty to look after this part of the world, not just the one million plus patients who come to hospital for treatment.
To limit the effects of climate change, the trust plans to reduce our carbon footprint by a significant amount, from 6.5 tonnes per person each year to under two tonnes by making fundamental changes to the way our hospitals and our staff work.
The trust will be switching to sustainable suppliers and only using suppliers who disclose their carbon emissions, helping not just the environment but the local economy.
Staff will be encouraged to use more sustainable modes of transport, from electric vehicles to cycling and walking to work to improve the air quality around our hospitals.
More efficient ways of heating and lighting are being used in all new buildings as part of the major construction work under way at both main hospitals.
The trust has just received the £12.6m grant from the Department for Business Energy and Industrial Strategy as part of its Public Sector Decarbonisation Scheme to support its new green agenda.
Alex Best, Head of the trust’s Capital Development department, said: “The LED lighting upgrade is one of a number of projects being delivered over the next few months including the development of solar ground array, insulation to buildings and decarbonisation schemes such as heat pumps, all of which will have a positive impact on our estate.”
Duncan Taylor, Director of Estates, Facilities and Development at the trust, said: “It’s been a difficult year for the NHS but even during the pandemic, we’re keen to do what we can to prevent climate change and start to reduce our carbon emissions.
“The funding from the Public Sector Decarbonisation Scheme will really help by allowing the trust to deliver this multi-million pound decarbonisation project, which includes the installation of solar panels and heat pumps and other energy efficient equipment upgrades.”


 The team has helped women in labour and their partners, supporting them as they deal with the added anxieties and stresses of bringing a new baby into the world during a pandemic.
The team has helped women in labour and their partners, supporting them as they deal with the added anxieties and stresses of bringing a new baby into the world during a pandemic.



 She said: “I’d like to say a huge thank you to all Ward 16 staff and to all who have joined us during our pandemic experience.”
She said: “I’d like to say a huge thank you to all Ward 16 staff and to all who have joined us during our pandemic experience.”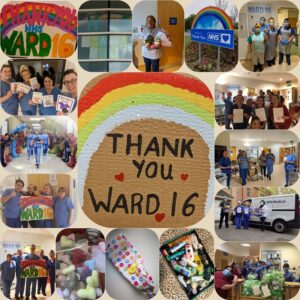 In a direct message to her team, Melanie Jopling said: “You should be extremely proud you have worked amazingly and professionally throughout, adapting to all challenging changes .
In a direct message to her team, Melanie Jopling said: “You should be extremely proud you have worked amazingly and professionally throughout, adapting to all challenging changes .




 James Illingworth, the trust’s Research and Development Manager, said: “Over the last 11 months, healthcare organisations across the world have turned to research for answers in the fight against the Covid-19 pandemic. Our trust is no exception.
James Illingworth, the trust’s Research and Development Manager, said: “Over the last 11 months, healthcare organisations across the world have turned to research for answers in the fight against the Covid-19 pandemic. Our trust is no exception.
 Chief Nurse Beverley Geary said: “We understand how difficult it has been for people not to be able to see their loved ones. We thank people for understanding the safety of our patients has been – and continues to be – our priority during the pandemic.
Chief Nurse Beverley Geary said: “We understand how difficult it has been for people not to be able to see their loved ones. We thank people for understanding the safety of our patients has been – and continues to be – our priority during the pandemic.