Chris Long, Chief Executive of Hull University Teaching Hospitals NHS Trust, said 3,000 outpatient appointments a day were cancelled for four months along with routine surgery and hospital procedures at Hull Royal, Castle Hill Hospital, Hull Women and Children’s Hospital and Hull Eye Hospital.
Now, with the initial peak of the virus over, all hospitals are attempting to resume surgery, outpatient clinics and other services against the backdrop of the still-present virus, the constraints of social distancing and the requirement of Personal Protective Equipment (PPE).
In a direct video message to patients, Mr Long said: “I am really, really sorry. None of us want to see people in pain or want to see people suffering or having to wait.
“We are doing everything that we can to try and get through the work. We are doing everything we can to change way that we do things and we are looking at how to work with partners to do some things differently.
“We are absolutely focused on getting you treated as soon as we possibly can.”
More than 44,000 people have lost their lives to the virus in the UK, including 203 at Hull Royal and Castle Hill since March 19. More than 500 people with the virus have been discharged from hospital and around 24 patients with either confirmed or suspected Covid-19 are still receiving treatment.
Mr Long said the trust was currently “running to stand still” to maintain hospital services after the cancellation of all but life or limb saving surgery following the lockdown in March.
He said: “Due to the constraints and the need to maintain social distancing, due to the need of our staff changing their PPE frequently, our productivity has gone right down.
“We can’t see the volumes of patients we normally do and I’m afraid the consequences are people are going to have to wait longer for operations and other procedures.
“Everything but urgent life-saving or limb-saving operations had to be cancelled while we prepared. We see about 3,000 outpatients every day so it doesn’t take long for that to build up.
“Due to the reduction in productivity, it is going to take years to recover. I’m afraid there is not going to be a quick fix.”
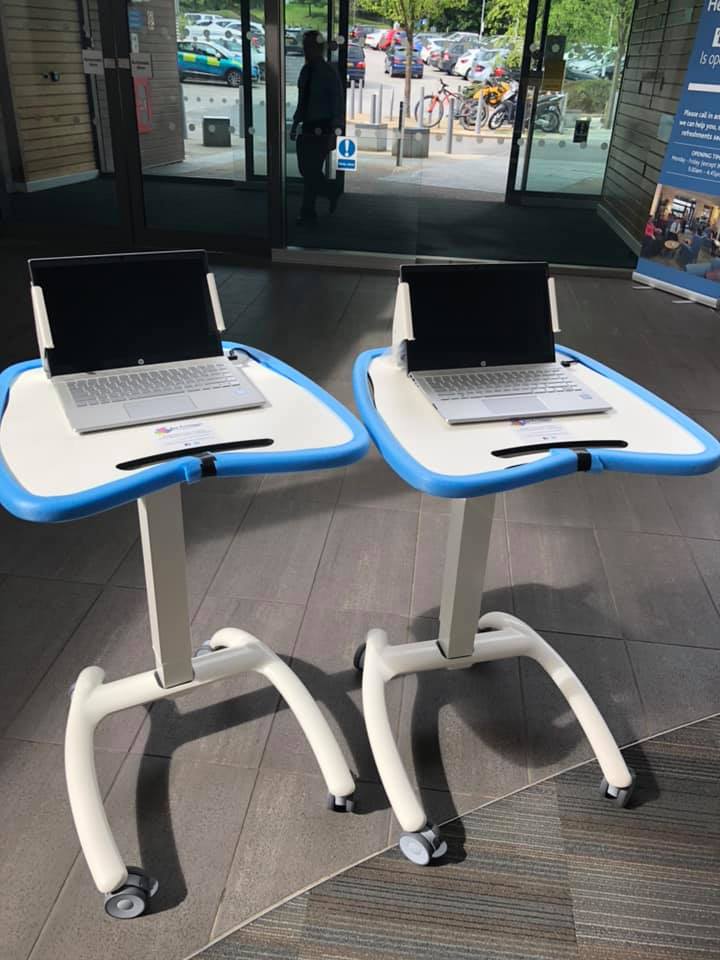
Video and telephone consultations have been introduced in some services where appropriate to help reduce waiting lists and prevent people making unnecessary trips to hospital. Clinical teams work together to prioritise patients awaiting treatment and the trust is working with Spire Hospital so those most in need are treated.
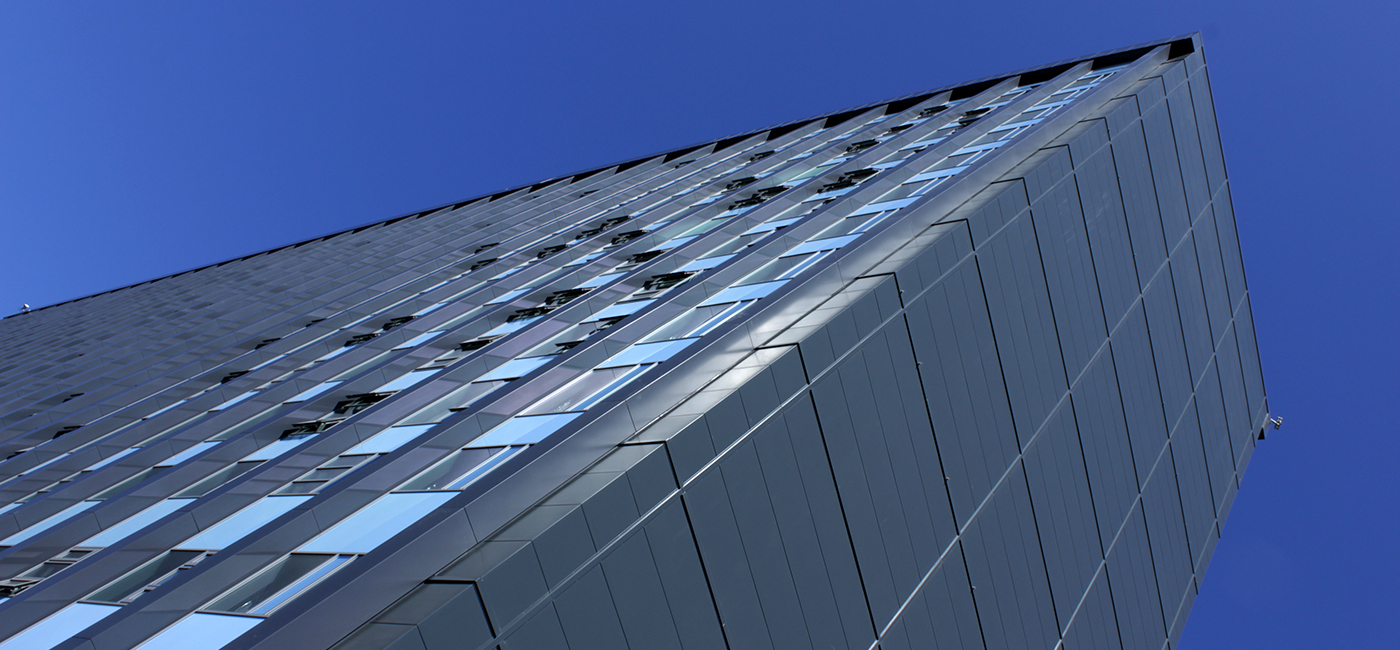
Mr Long said the trust was now preparing for a potential second wave later in the year, with two new wards being constructed at the back of the tower block at Hull Royal Infirmary to care for patients with the virus.
The Chief Executive has appealed to the public to continue following social distancing, hand hygiene and not to come to hospital if they are showing any symptoms of the virus including a dry, continuous cough, a temperature or the loss of their sense of taste or smell.
He also paid tribute to the trust’s 9,000-plus workforce for working throughout the pandemic to ensure they could care for those most in need.
He said: “They have been absolutely magnificent.
“they have thrown themselves into it. People have put themselves at risk without any thoughts for themselves.
“They have done everything that they can to make sure our patients are looked after properly and cared for properly. They have worked as a team brilliantly and it has been flat out.
“What I cannot emphasis enough is just how long this has been going on for. Having come out of winter, they went straight into this and they are still hard at it.
“Everyone should be really proud of their NHS Staff. I couldn’t be prouder of them.”






 Hull University Teaching Hospitals NHS Trust discharged its 500th patient this week after confirming the first two cases of the virus in Britain in January.
Hull University Teaching Hospitals NHS Trust discharged its 500th patient this week after confirming the first two cases of the virus in Britain in January.