Paediatric emergency consultant Dr Liz Herrieven has told how her teenage daughter’s dual diagnosis of Down’s syndrome and autism has had a positive impact on her life.
Dr Herrieven has taken part in the Shifting Perspectives Podcast to talk about life with 13-year-old daughter Amy.
She explained how life-threatening illnesses when Amy was younger has helped her role as a consultant in emergency medicine at Hull Royal Infirmary, given her great insight into what it’s like to be the parent of a seriously ill child.
In a message to parents of children with Down’s syndrome, Dr Herrieven said: “Take one step at a time, particularly in the early days. Be kind to yourself. It’s ok to feel things are awful, it’s ok to be sad and it’s ok to have that grieving process.
“You will get through the other end. There will be good days and there will be bad days but, in the end, you will have far more good days than bad.
“Your family may not look like the wonderful family on the front of all the parenting magazines but, actually, your family is your family – unique and special to you.
“Don’t worry what anyone else is doing.”
The podcasts have been produced by the Down’s Syndrome Association and hosted by photographer Richard Bailey to share stories of people with Down’s syndrome as well as of their families and carers.
Amy was born 10 weeks early and spent her first few months in neonatal intensive care. In her early years, she spent weeks in high dependency and intensive care units with life-threatening illnesses including severe chest infections, pneumonia and sepsis.
Dr Herrieven said: “I was so used to being on the other side, being the one that makes the decisions.
“Suddenly, I had lost control and it was my small child lying there. That taught me a massive amount of what it’s like to be on the receiving end of challenging news.”
Amy was diagnosed with autism at the age of eight, enabling her family to make adjustments to make life easier by reducing her levels of anxiety.
While looking after Amy’s needs, Dr Herrieven and her husband ensure Amy’s eight-year-old brother Toby has time for fun and the family sticks to familiar routines to help Amy such as going to the same place on holiday every year.
“Amy is Amy and Down’s syndrome is part of her,” Dr Herrieven said.
“Although we have changed our expectations, we still manage to have a really good family life.”
Dr Herrieven realised being Amy’s mum could help other medical professionals in the treatment of people with Down’s syndrome.
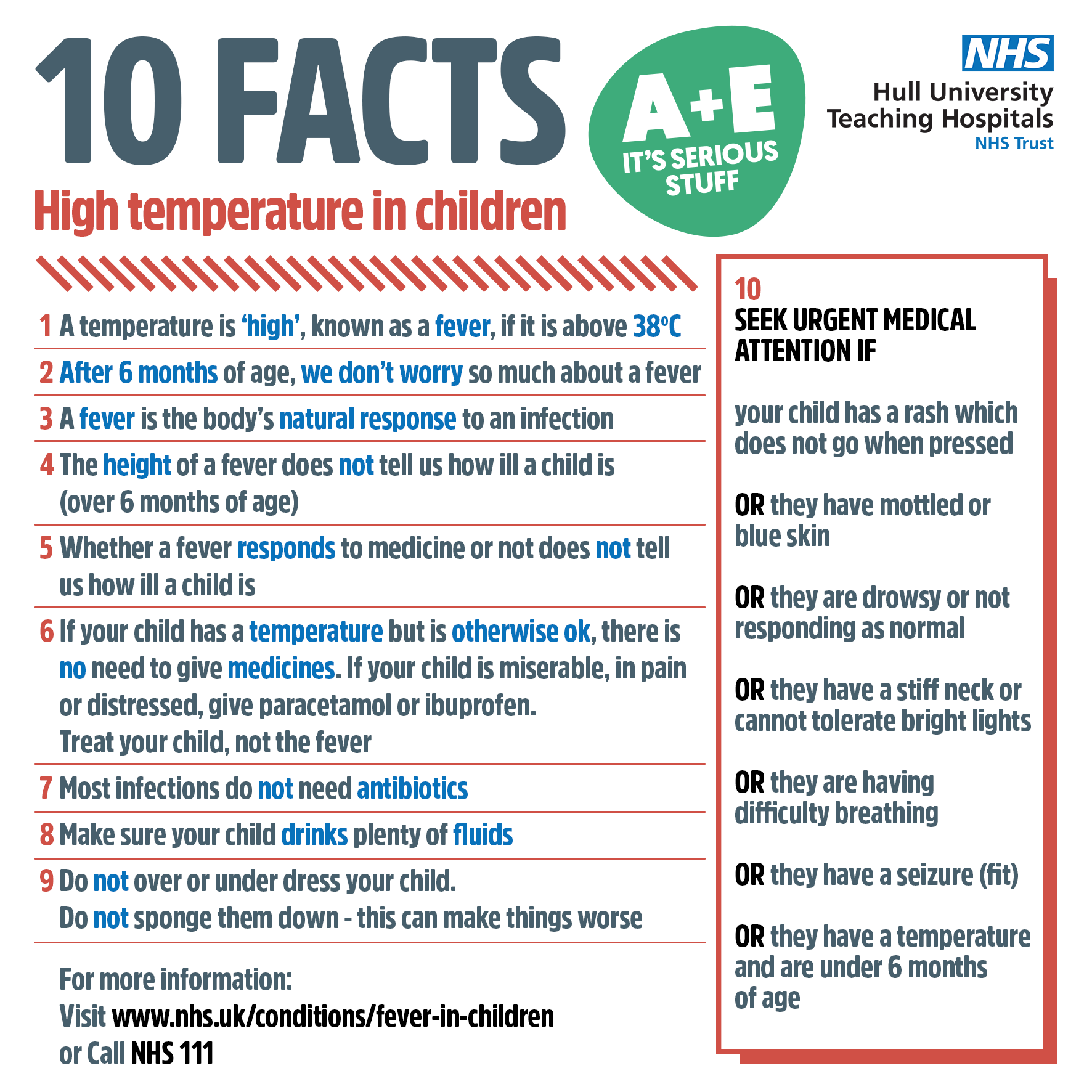
Together with Linda Dykes, an emergency medicine consultant and GP in Bangor, she has produced an infographic for other clinicians with top tips on triaging and treating children with Down’s syndrome.
The infographic has received 100,000 hits and has led to Dr Herrieven blogging for the Royal College of Emergency Medicine as well as speaking at a conference of paramedics.
Dr Herrieven is also working hard to challenge “diagnostic overshadowing” when the judgement of medical professionals is clouded by a person’s condition.
She said: “As medical professionals, we tend to use scoring systems and lists of signs and symptoms to see how sick a person is but sometimes, these things don’t work and that’s particularly true of people with Down’s syndrome.”
Dr Herrieven called on doctors to consider “soft signs” where a person’s behaviour has changed, such as they are not interested in something which normally engages or distracts them.
She said: “Families are probably better than medical professionals at recognising these things and it will be different for every person.
“We need to start listening to these things families are telling us about when someone’s behaviour is different.”
You can hear Dr Herrieven’s podcast through the Down’s Syndrome Association website.