Rugby star Shaun Lunt is appealing to people to “think sepsis” after he developed the life-threatening condition following a rugby tackle.
Shaun, former captain of Hull KR, suffered an abscess in his spine following the tackle during a game in August 2018 which became infected and he developed sepsis.
Now, as the first anniversary of his battle for survival approaches, Shaun, 32, is supporting Hull University Teaching Hospitals NHS Trust to mark World Sepsis Day on Friday.
He said: “None of us want to make a fuss but there’s a risk that we don’t take this seriously enough.
“People are scared to look stupid if they mention sepsis but we need to be more cautious and think sepsis, whether they work in the hospital, are looking after someone or feel the worst they’ve ever felt in their life.
“You can lose a limb affecting the rest of your life or even lose your life if you don’t.”
Sepsis is when your body reacts in a toxic, life-threatening way to an infection that can lead to tissue damage, organ failure or death.
Shaun’s health began to deteriorate after he suffered the back injury during the game in August 2018. He was taking painkillers but, by the end of September, he had gone to different hospitals twice as his condition worsened.
One morning, unable to get up off the floor between his bed and his wardrobe, he knew he had to get to hospital immediately.
“I’m one of those that don’t like to make a fuss but I phoned my wife Grace and said I needed to go to hospital,” he said. “It was the worst I’d ever felt.”
Shaun was taken to Pinderfields Hospital in Wakefield where doctors initially suspected bacterial meningitis before he was diagnosed with the abscess on his spine and sepsis.
After eight days, Hull KR arranged for him to be transferred to Nuffield Hospital in Leeds for 12 days. He was then given antibiotics intravenously through a PICC line for a further six weeks.
Shaun said: “When I came out, I thought I’m getting better and, a couple of months later, I went to watch a football game with one of my friends. He told me how bad sepsis was and how someone he knew had died from it.
“I was quite naïve about it and hadn’t realised how serious it had been.”
Although he recovered enough to return to playing in March, his battle was far from over.
Shaun struggled with post sepsis syndrome, a condition affecting around half of sepsis survivors. It can leave people with depression, loss of self-esteem, debilitating muscle or joint pain and hallucinations.
“About 10 weeks after being in hospital, everything hit me like a tonne of bricks,” he said. “I’d come off the medication but that was when the real battle began.
“Post sepsis syndrome was an absolute nightmare and the worst thing was that no-one had warned me what was to come.”
His love for wife Grace and their two sons, Noah, 7, and four-year-old Jude helps Shaun find the strength to continue his recovery and he rejoined Leeds Rhinos on loan in June.
He missed Noah’s seventh birthday because he was admitted to hospital just three days before on September 27 and then spent days in quarantine so this year’s celebration will be extra special.
He understands how close those who love him came to losing him and he’s determined to return to full health.
“I’m not afraid or ashamed to admit I’m still not 100 per cent,” he said. “It’s just an on-going process but I know I’m getting better.
“In the beginning, I was lucky to get a couple of good hours because every day was a bad day. Then it was one good day in a week. Now, I maybe have a tough day every couple of weeks but I know what it’s about now.
“I can talk to my wife and we know it’s all part of the healing process and something I have to go through.”
Hull’s A&E department sees at least 50 patients with sepsis every month while other people already in hospital with other illnesses and injuries can also develop sepsis.
Since the trust introduced its sepsis team in 2015 as part of a national initiative to drive up survival rates, around 90 per cent of patients brought to A&E with signs of severe infection are now screened for sepsis.
Around 80 per cent of those diagnosed with sepsis receive life-saving antibiotics within an hour.
Donna Gotts, Clinical Nurse Specialist in Sepsis at Hull Royal Infirmary and Castle Hill Hospital, said: “We are so grateful to Shaun for the work he is doing to help us spread the message.
“We need all health professionals to think sepsis and to be ready to take swift action so we can save more lives.
“In Hull, we’ve got a really good pathway which begins with Yorkshire Ambulance Service staff who can start the escalation pathway, alerting our Emergency Department so they’re ready for the patient arriving.
“This means that we can start the treatment for sepsis quickly. “
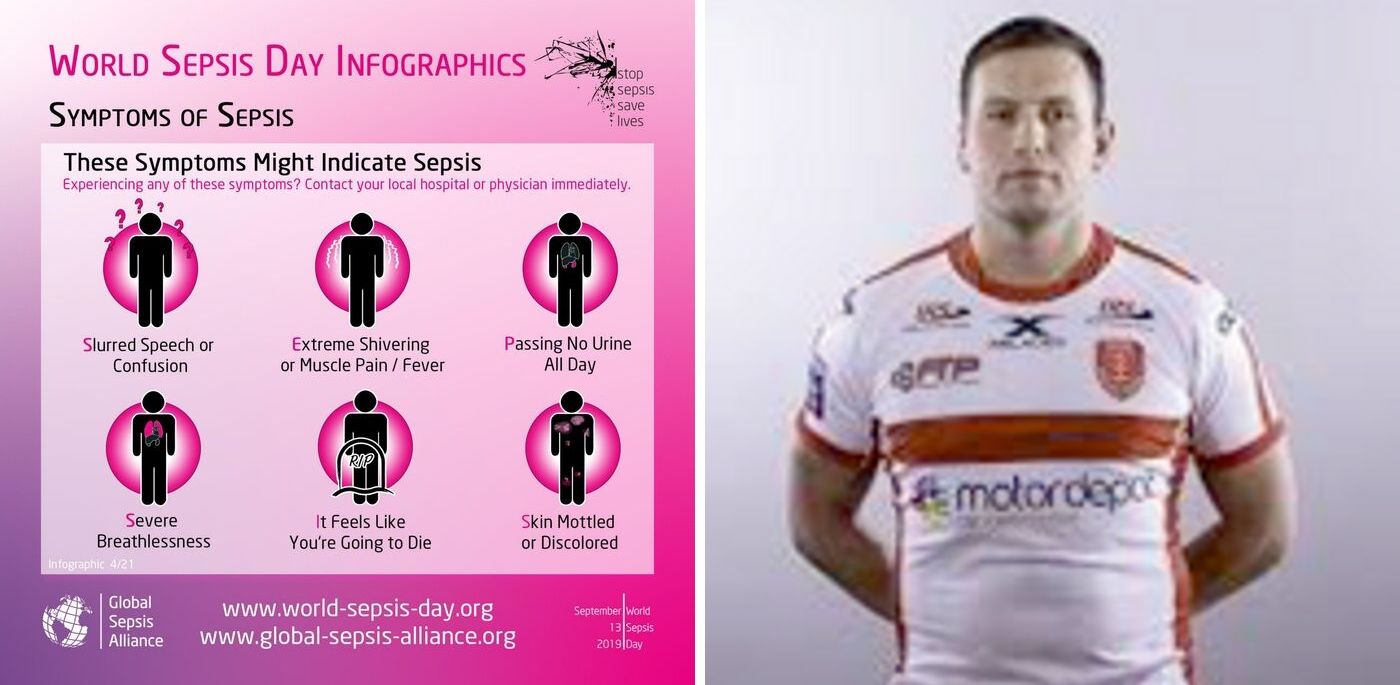
SIGNS OF SEPSIS
If your child is under five, call 999 or head straight for A&E if they have any of these symptoms – looks mottled or bluish, is very lethargic or difficult to wake, feels abnormally cold to the touch, is breathing very fast, has a fit or convulsion, has a rash that does not fade when pressed.
In older children or adults, early symptoms of sepsis may include a high temperature or low body temperature, chills and shivering, a fast heartbeat, fast breathing.
Symptoms of severe sepsis include feeling dizzy or faint, confusion or disorientation, diarrhoea, nausea and vomiting, slurred speech, severe muscle pain, severe breathlessness, less urine production than normal, cold, clammy and pale or mottled skin and loss of consciousness.