Non-urgent outpatient appointments and routine surgery at Hull’s hospitals will be postponed from today to allow staff to deal with the COVID-19 outbreak.
Hull University Teaching Hospitals NHS Trust is cancelling some elective procedures and outpatient appointments following a national announcement by NHS England to free up 12,000 to 15,000 hospital beds around the country.
However, emergency operations and admissions, cancer treatment and clinically urgent work will still go ahead.
Cancelling non-urgent operations and outpatient appointments from today will free up staff to undertake training, beds, theatres and recovery facilities ahead of the predicted COVID-19 peak in a few weeks.
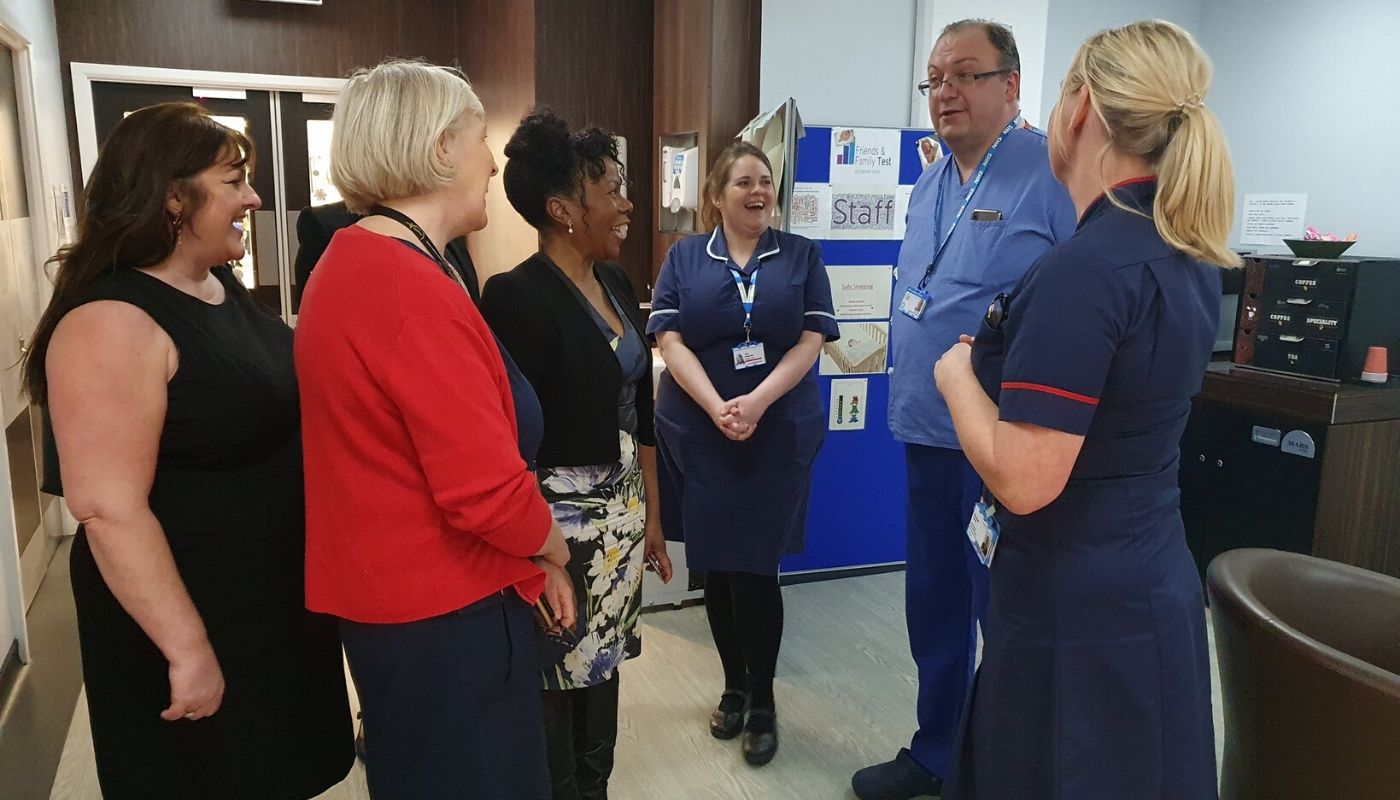
Jacqueline Myers, the trust’s Director of Strategy and Planning, said: “As the Chief Medical Officer has stated, NHS services are likely to come under intense pressure as the coronavirus spreads. We need to ensure that we have as many beds available as possible to care for patients with severe respiratory problems when the number of infections peaks.
“Therefore, in line with well-established plans for situations like this, every hospital in England has now been asked to suspend all non-urgent elective operations for at least three months, with some other procedures likely to be rescheduled so we can train our staff and adapt certain areas.
“Urgent and emergency cases and cancer treatments will be carrying on as normal, but we know many people waiting for treatment will be disappointed or worried and we will be contacting everyone affected as soon as possible.”
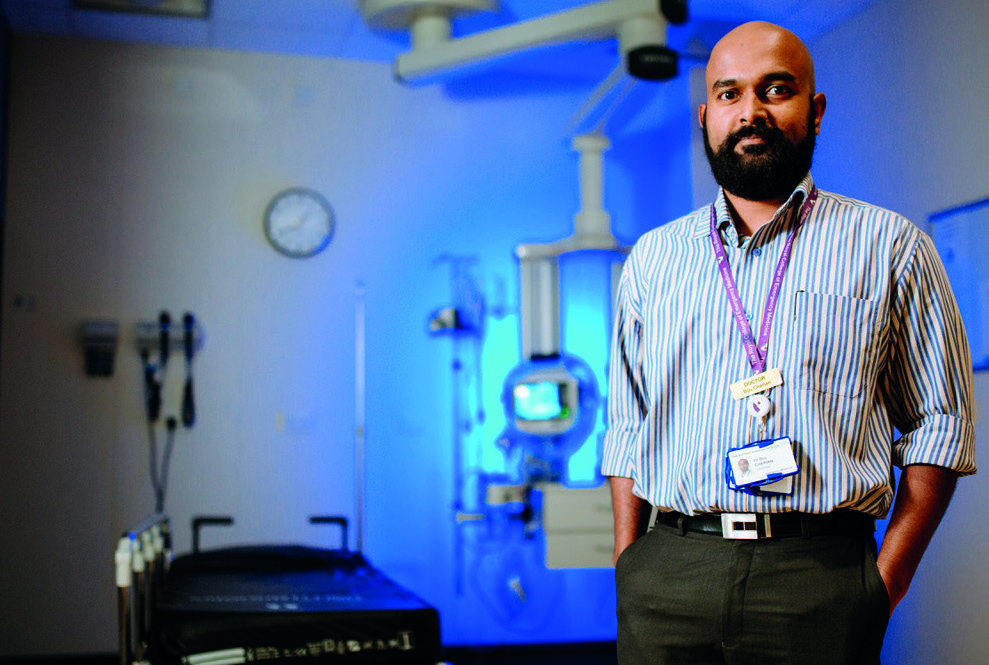
The trust’s patient admin team are working as fast as possible to alert patients who have appointments over the next few days and weeks and are appealing to the public not to call the hospital about their appointments.
If your appointment is within the next seven days and is to be cancelled or changed to a telephone consultation, you will receive a telephone call from the Patient Admin team and a follow-up letter.
If your appointment is more than seven days from now, you will receive a letter if your appointment is to be cancelled or changed to a telephone consultation.
Some patients will still be required to attend to continue treatment so, if you do not receive a letter or a phone call, please turn up for your appointment as normal.