Businessman and philanthropist Dr Assem Allam is to donate almost £8m to Hull University Teaching Hospitals NHS Trust for the provision of world-class treatment and research facilities at Hull Royal Infirmary and Castle Hill Hospital.
The multi-million pound donation will create a centre of excellence in the care and treatment of patients with diabetes and metabolic bone diseases such as osteoporosis, a new facility to treat digestive diseases and a major expansion of robotic surgery. It will also provide additional funding for the Molecular Imaging Research Centre developed by the Daisy Appeal to help patients with cancer, heart disease and dementia at Castle Hill Hospital.
Major investment on this scale has not been seen in the city since the times of industrialist and philanthropists Sir Thomas Ferens and Christopher Pickering and will be matched by the hospital trust to create the £16m transformation of healthcare benefitting tens of thousands of patients.
Work will begin on the new projects early in 2020, with the centres up and running by the end of 2021.
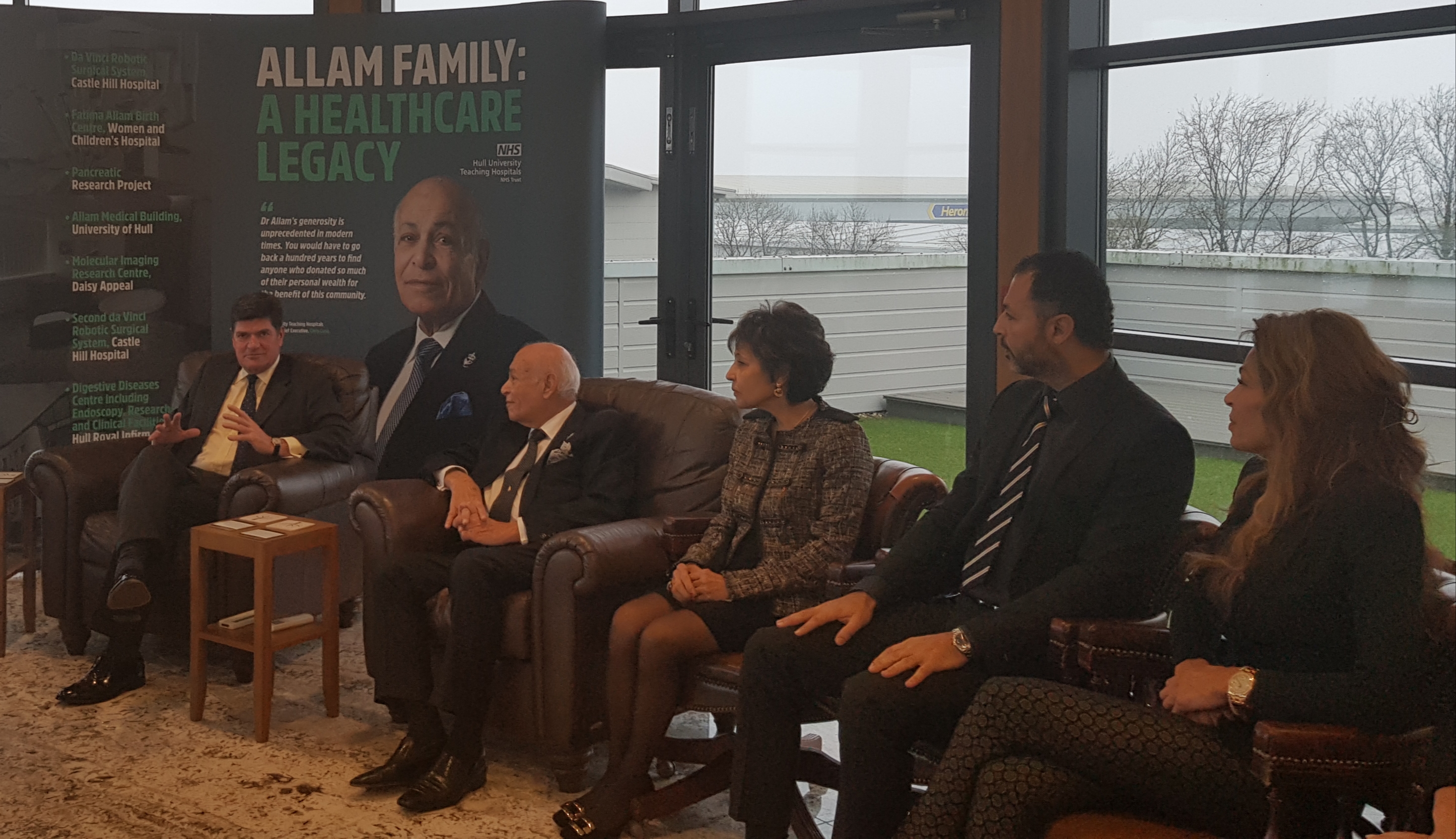
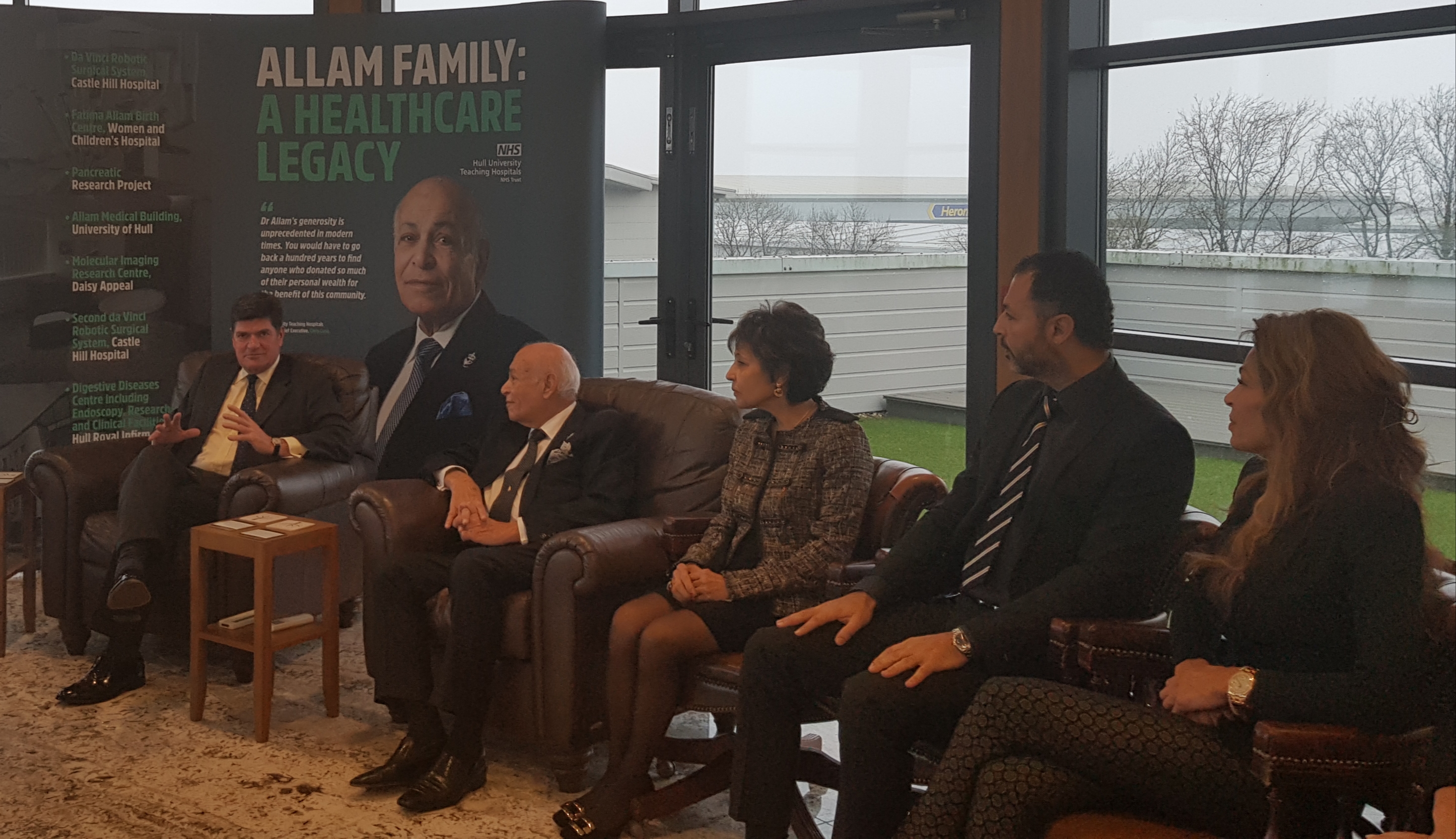
Trust Chief Executive Chris Long thanks Dr Allam and his family for their generous donation
Dr Allam said: “I moved to this part of the UK in 1968 and I am passionate about this region and the people of East Yorkshire.
“People have always been very good to me and my family and we are grateful to them for their support and kindness. For those reasons we want to demonstrate our gratitude by investing in healthcare facilities which will bring greater longevity to people’s lives and benefit not just patients but their families and loved ones also.
“I believe that, in particular, we must invest in research and development, which will improve recruitment to our hospitals at the same time as generate further investment in this great city and ultimately enable us to develop new and innovative treatments for patients.”
Not only will the Allam family’s donation provide modern buildings in which to care for patients, it also strengthens Hull’s growing reputation as a global player in research, enhancing research and teaching facilities in endocrinology and diabetes and a vascular surgery diabetes research facility at Hull Royal Infirmary.
Additional education facilities to support the training of medical students in the Hull York Medical School will also be created as part of the new building proposed for Hull Royal Infirmary.
A new three-storey building housing clinical endoscopy, research and teaching facilities for the treatment of digestive diseases will also be built at Castle Hill.

Dr Assem Allam
The latest donation from Dr Allam and his family underlines their significant and outstanding contribution to the improvement of health facilities in Hull and the East Riding of Yorkshire.
- A 2014 donation enabled the development of robotic surgery at Castle Hill Hospital, significantly improving the procedures to undertake prostate surgery and its use has subsequently extended to include major gynaecological surgery, bowel cancer surgery and thoracic surgery. A second Da Vinci Surgical Robotic System and a major expansion of robotic surgery capacity can now be created, thanks to the Allam family donation.
- The development of the Fatima Allam Birth Centre in April 2017 at Hull Women’s and Children’s Hospital. Since opening in April 2017, the midwifery-led unit has cared for more than 1,000 families while their babies are born
- Sponsorship of a pancreatic research project, undertaken jointly by clinical and scientific research staff at the trust and the University of Hull.
- A major contributor to the Molecular Imaging Research Centre being developed on the Castle Hill Hospital site by the Daisy Appeal. The prime aim of this development is to improve the clinical diagnosis and treatment of patients with cancer, cardiac disease and neurological conditions.
- And, in 2018 Her Majesty the Queen opened the £28m Allam Medical Building at the University of Hull, made possible thanks to a £7m donation from Dr Allam.
Trust Chief Executive Chris Long has described Dr Allam’s generosity as unprecedented in modern times.
He said: “With this latest philanthropic gesture, Dr Allam is unrivalled in terms of the investment he has made into healthcare facilities in modern times. You would have to go back a hundred years to find anyone who donated so much of their personal wealth for the benefit of this community, in terms of their health and the care we provide for patients.
“We are extremely grateful to Dr Allam for this latest donation which will leave a legacy for patients in this region for generations to come.”
Enabling works for the diabetes scheme at Hull Royal Infirmary are already underway. Once completed in January 2021, diabetes, endocrinology and metabolic bone disease services will be re-located from their current home in the Brocklehurst building on Anlaby Road to a modern facility next to Women and Children’s Hospital. While patients would directly benefit from a much improved environment, the overall aim is to enhance and develop world-class endocrinology and diabetes research facilities at Hull Royal Infirmary and attract staff and funding streams into our region.
Development of the digestive diseases and endoscopy facility at Castle Hill Hospital will significantly increase the scale of clinical accommodation available and ensure that the trust has the capacity to effectively respond to the continued growth in demand for these services. This building will also provide dedicate research space and a new purpose-designed facility for the Hull Yorks Endoscopy School, which is centred on the hospital.
Investment proposals in robotic surgery are a less developed at this stage but with the finances secured Hull University Teaching Hospitals is confident that they can now progress with the detailed planning work required.
David Haire, Project Director Fundraising at the trust, said: “Once again, this is a significant donation from Dr Allam and his family to the trust, and our city and wider region.
“Sometimes, his generosity is taken for granted but that certainly isn’t the case from our perspective. Everyone at the trust, along with those patients and their families who will benefit from this continuing patronage, is very grateful to Dr Allam and we look forward to developing these new schemes into facilities of which all can be extremely proud.”










 Dr Mohammed said: “This will be my second visit to the Gambia and I will be part of a team of health professionals from different hospitals all over the UK and beyond.
Dr Mohammed said: “This will be my second visit to the Gambia and I will be part of a team of health professionals from different hospitals all over the UK and beyond.