Castle Hill team becomes first in country to achieve service quality standard
A team of healthcare science professionals in Cottingham have become the first in the country to achieve a new standard which assures cancer patients of quality care.
Safety, treatment planning and equipment maintenance were among the areas reviewed as the Radiotherapy Physics Team at Castle Hill Hospital took part in the independent two-year pilot Medical Physics and Clinical Engineering (MPACE) accreditation scheme. MPACE independently reviews all aspects of healthcare science which underpin the radiotherapy treatment provided to patients.
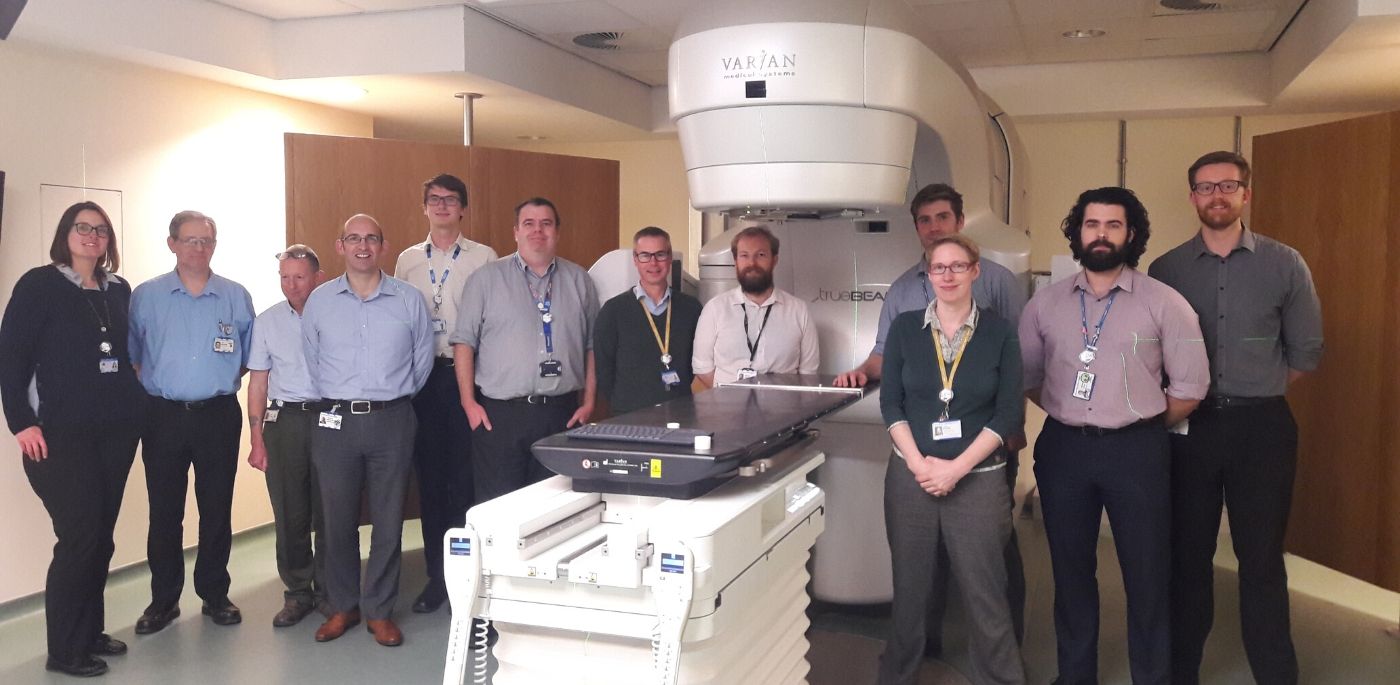
Now the 36-strong team are the first radiotherapy physics team in the country to achieve service standard BS 70000:2017, assuring patients around the quality and safety of the service they’re receiving and the competence of staff delivering treatment.
Pete Colley, Consultant Physicist Lead for Radiotherapy at Hull University Teaching Hospitals NHS Trust said:
“Our team jumped at the chance to take part in the MPACE accreditation scheme when it was offered to us back in 2017.
“This independent assessment has looked at everything from how we staff our service to the upkeep of our equipment and the design of patients’ treatment plans.
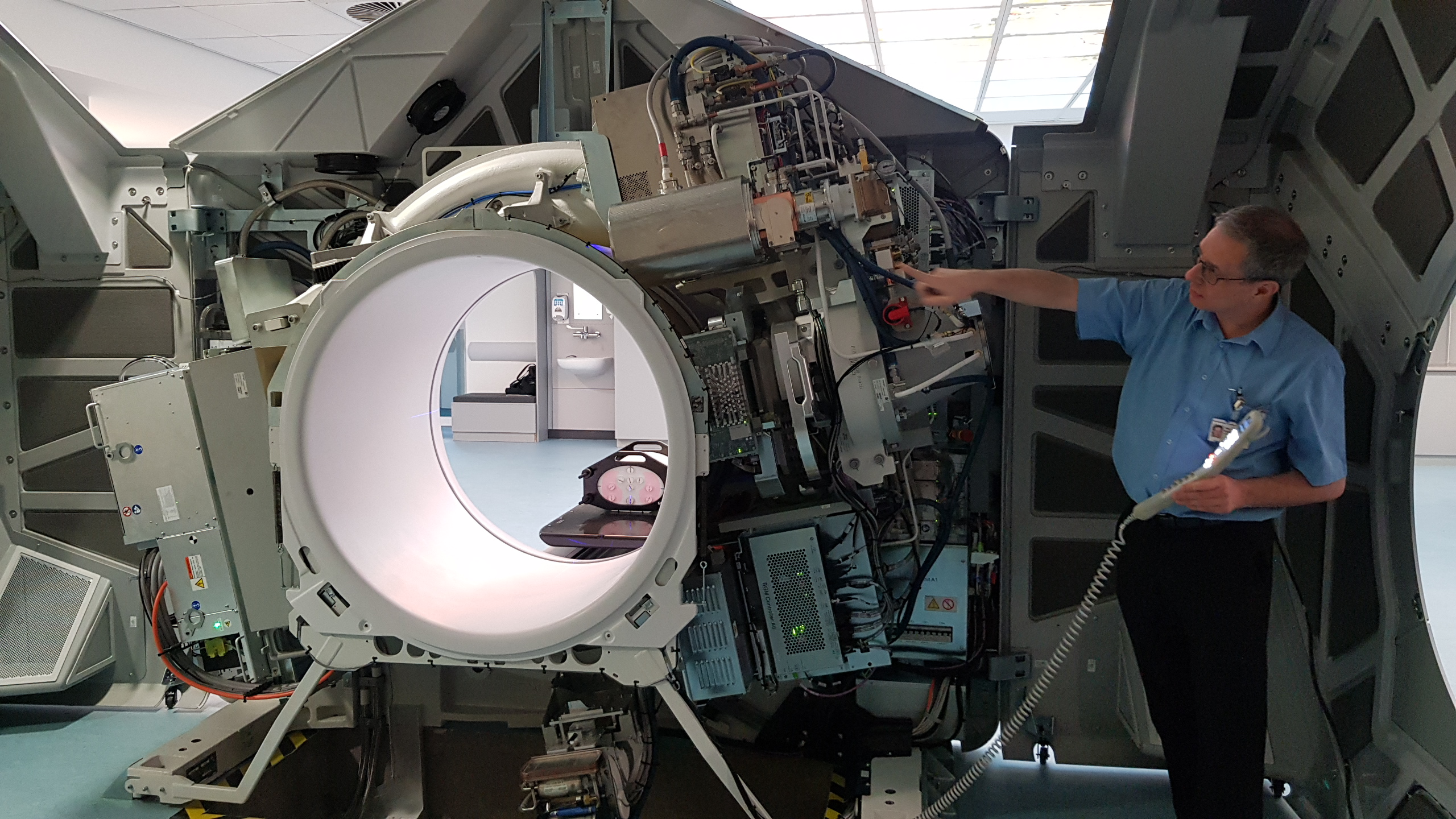
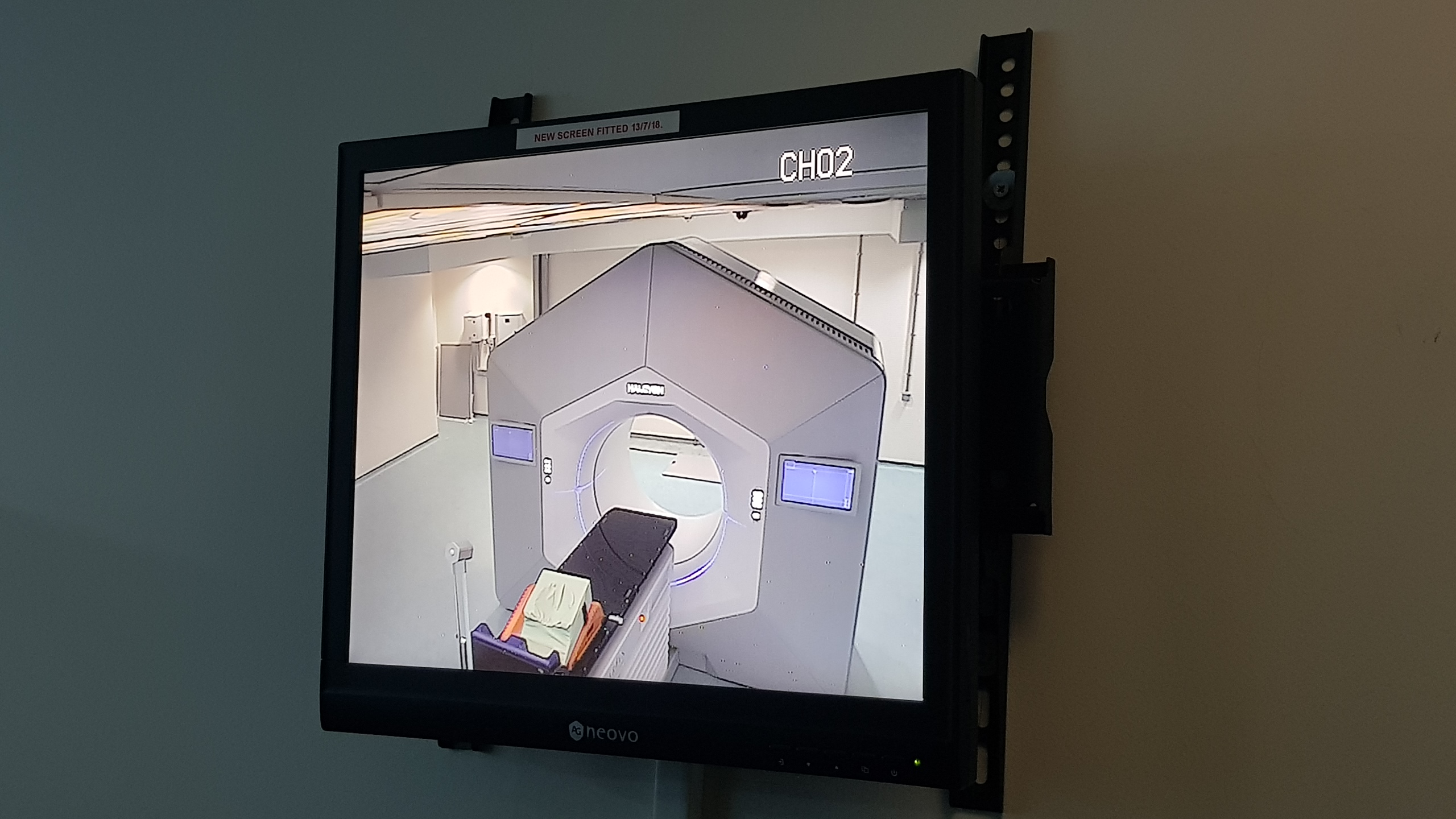
Clinical technologist Neil Bastiman at the recent launch of the Varian Halcyon linear accelerator
“We know we have the best interests of our patients at heart, but now we have been awarded MPACE accreditation, this is how we know we are doing a good job for our patients.”
Around 170 patients receive radiotherapy treatment for cancer every day at the Queen’s Centre at Castle Hill Hospital, with some patients receiving daily radiotherapy sessions for up to a month at a time.
Explaining the reasons why Hull University Teaching Hospitals took part in the MPACE pilot, Richard Whitlam, Quality Manager said:
“Our medical physics department has been ISO 9001 certified for many years, but we were looking to increase levels of patient and professional assurance in the competence of our staff and quality of our service.
“Being UKAS accredited under the MPACE scheme means we now have independent evidence to show that our staff are competent and that we deliver a high quality service focused on putting patient care first.
“This can only serve to reassure our patients at what can often be a worrying or stressful time for them, and it’s a real boost for the radiotherapy physics team who have worked so hard to get to this point.”