Got a tattoo? Been abroad to get your teeth fixed or had breast implants or a nose job overseas?
Between 4,000 and 6,000 people in East Yorkshire are thought to living with hepatitis C, many of them not suspecting they have a virus which could cause liver failure or cancer.
Now, a specialist team based at Castle Hill Hospital is heading into Hull’s housing estates and GP practices this year to screen people for the virus as part of the plan to eradicate hepatitis C by 2025.
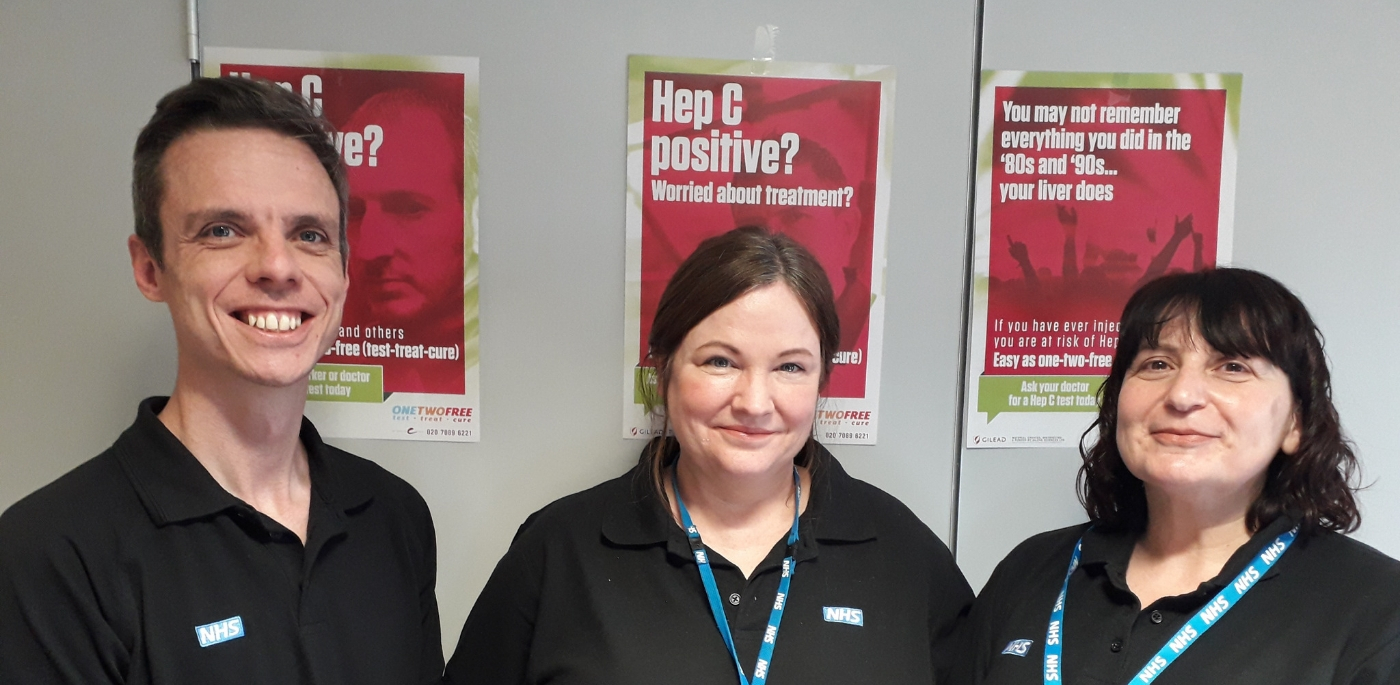
From left Martin Lewis, Hattie Deverell and Alison West
Specialist Nurse Martin Lewis said: “Lots of the people we see tell us they don’t know how they’ve caught hepatitis C but it turns out they’ve got tattoos or they’ve been abroad on ‘health care holidays’.
“There is a lot of stigma attached to hepatitis C because of its links to intravenous drug use but you could have caught it if your tattoo was done with a dirty needle or the health facility where you underwent your procedure did not practice the same standards of hygiene as the NHS.
“Some people tell us they only engaged in high-risk behaviour once but that’s all it can take to contract hepatitis C.
“We want people to know there’s nothing to be ashamed of and we are here to help them. Treatment is much better now than it was in the past and the medication we can prescribe gets rid of the virus in 94 per cent of cases.
“But to help people, we need them to come forward for screening.”
What is hepatitis C?
Originally discovered in the 1980s, it was first known as non-hepatitis A and B before it was named hepatitis C in 1989. A screening programme was introduced in 1991 to check all blood donations for hepatitis C.
Hepatitis C is a blood-borne virus and, over time if left untreated, can cause significant liver damage.
There is no vaccine to stop people catching hepatitis C but a course of medication can get rid of it.
How do you contract hepatitis C?
Hepatitis C can only be contracted through blood. You can’t get it from hugging, kissing, toilet seats or from sharing food and drink and utensils.
However, you can catch it if you’ve had tattoos from dirty needles or medical and dental treatment abroad or privately where hygiene standards may not be to NHS standards.
Unprotected sex, high-risk sexual behaviour, having a blood transfusion before 1991, intravenous drug use and sharing needles or sharing hygiene products such as wet razors and tooth brushes are all known risk factors which could lead to the transfer of blood.
How many people are affected by hepatitis C?
Around 71 million people have hepatitis C and it claims the lives of 400,000 people every year when it develops into liver cirrhosis and liver cancer.
Estimates suggest between 4,000 and 6,000 people in Hull and its surrounding areas have hepatitis C although many will be unaware they have the condition.
What are the symptoms of hepatitis C?
Studies have been unable to provide conclusive evidence on symptoms directly attributed to hepatitis C.
However, they can include tiredness, depression, loss of appetite, mood swings, headaches, flu-like symptoms, bloating, nausea, joint and muscle pain, itchy skin and jaundice.
The problem is people are unlikely to link any of these to a medical condition until symptoms of liver failure start to appear – and that can take 15 to 30 years.
How can it be treated?
In the past, treatment for hepatitis C was difficult. Drugs had many side effects, only worked in around 50 per cent of patients and treatment could take almost a year to complete.
However, new antiviral medication has now been developed and is equally effective for all six types of hepatitis C.
People are given one to three tablets a day, tailored to their specific type of hepatitis C, and treatment lasts between eight to 16 weeks. Unlike before, the new treatment is 96 per cent effective for all six types of hepatitis C and with far fewer side effects.
What’s happening in East Yorkshire to tackle the problem?
Hull is one of 22 “Operational Delivery Networks” set up in 2015 to treat people with the condition and increase screening rates to ensure people with hepatitis C are identified and given treatment to prevent them becoming seriously ill in the future.
The six-strong team working with are two Infectious disease consultants and two heptologists is currently treating around 140 patients a year.
Although based at Castle Hill Hospital, three specialist nurses – Martin Lewis, Alison West and Hattie Deverell – work in the community alongside GP practices, prisons and drug and alcohol services to reach known high-risk groups.
However, they now plan to extend outreach work into housing estates to screen people who may have no idea they have the virus.
Each person is then reviewed by the multi-disciplinary team to ensure they receive the best, most appropriate and most cost-effective treatment available.
How can you find out if you have hepatitis C
It’s easy to find out if you have hepatitis C. Your GP or a screening centre can arrange for a blood test or you can have a finger prick test similar to the tests used to monitor blood sugar levels. Results are usually known within two weeks.
Where can I go to be screened?
At the moment, you can get screened, make an appointment or undergo treatment at some GPs, Renew in Beverley Road in Hull, William Booth Hostel in Hull.
Inmates at HM Prisons, Hull and Humber, can also be screened for hepatitis C because they are a high-risk group.
Screening is also available through the East Riding Partnership in Hull, Goole and Bridlington and the hospital team are planning to publicise more outreach clinics at GP surgeries and housing estates in the coming weeks.