They come in every age, shape, and size, and from many different backgrounds. Some aim to develop their skills, while some come to share their talents. Some seek friendship, while others simply want to give back to their community.
What unites all of the 650 volunteers working across NHS Humber Health Partnership’s five different hospitals* is the desire to help others.
This week, 3 to 9 June, is Volunteers Week and there can be no better time to say thank you to those who help keep our hospitals in East Yorkshire and Northern Lincolnshire ticking over.
Volunteers are not just a support to patients and visitors, however, they’re a support to hospital staff too, with many ward staff describing their volunteers as ‘priceless’.
But if you think you know volunteering, think again, as those seen giving their time around our hospital wards and departments may just surprise you.
Did you know there are more than 200 young volunteers, known as Young Health Champions, working in local hospitals, many of whom are giving their time to learn essential skills on route to a healthcare career?
Others come to share their skills, whether it’s playing piano to lift the mood, helping people relax through complementary therapies, or providing advice on wigs to patients with cancer who have lost their hair during treatment.
Some of those walking the wards even come in a four-legged variety, with therapy dogs regularly visiting staff and patients on the intensive care units, stroke wards, paediatric wards, the Queen’s Centre for oncology and Castle Hill’s complex rehabilitation unit, and our neuro rehabilitation centre at Goole, to help people relax and act as a conversation-starter.
Rachael Hardcastle-Pearce is the Voluntary Services Manager for Hull Royal Infirmary and Castle Hill Hospital. She said: “Volunteering today is much more varied, with plenty of opportunities for people to share their skills and experience but also for people to gain experience which could help them in other areas of their own life or career.
“One of the things we’re really proud of right now is the links we’re forging with local partners, schools and colleges to give young people an insight into healthcare through voluntary placements. Not only will this help to build confidence at a young age and give school or college-leavers experience to put on their CVs, but as a potential employer, it gives us the opportunity to showcase the many and varied healthcare careers available and hopefully inspire the next generation of clinicians, scientists, and support staff.”
Julie Dobbs, Voluntary Services Manager, looks after those giving their time to volunteer across hospitals in Goole, Scunthorpe, and Grimsby. She said: “Our volunteers are an important part of our teams and complement the work of our paid staff to enhance the experience for our patients, carers, visitors, and staff. They bring a wealth of skills, experience, and energy to the roles they undertake, and we are so grateful for the time they give.
“Volunteers have a huge impact on our patient services, supporting staff by doing the little things that make a difference. We think they are amazing!”
Amanda Stanford, Group Chief Nurse for NHS Humber Health Partnership, said: “Volunteers donate thousands of hours each year to help support our patients, visitors and hospital staff. They each bring different skills and life experience, but the real gift they all bring to the team is the gift of time; the fact that our volunteers are able to chat with patients while nursing staff are busy or help direct a lost visitor while reception staff are helping others. These small things all add up to help deliver a much better experience for people across our hospitals.
“We’re proud to have so many volunteers on our team, and while we’re grateful for their support year-round, there’s no better time than the present, Volunteers Week, to say a public thank you on behalf of the whole Group to those who give their time to others.”
The hospitals’ voluntary service teams will be treating volunteers to a number of different activities to say thank you this week, including a walking tour of the city of Hull followed by coffee and cake, and a specially organised quiz night.
If you would like to know more about volunteering opportunities across our local hospitals, contact:
- Voluntary Service Team – Hull Hospitals
Tel: 01482 623089 / 07775 546434 or email r.hardcastle-pearce@nhs.net
- Voluntary Service Team – Northern Lincolnshire and Goole Hospitals
Tel: 03033 305577 or email nlg-tr.twvolunteering@nhs.net
Ends
Note to Editors
The five main hospital sites covered by NHS Humber Health Partnership are:
- Castle Hill Hospital Cottingham
- Diana, Princess of Wales Hospital, Grimsby
- Goole and District Hospital
- Hull Royal Infirmary
- Scunthorpe General Hospital













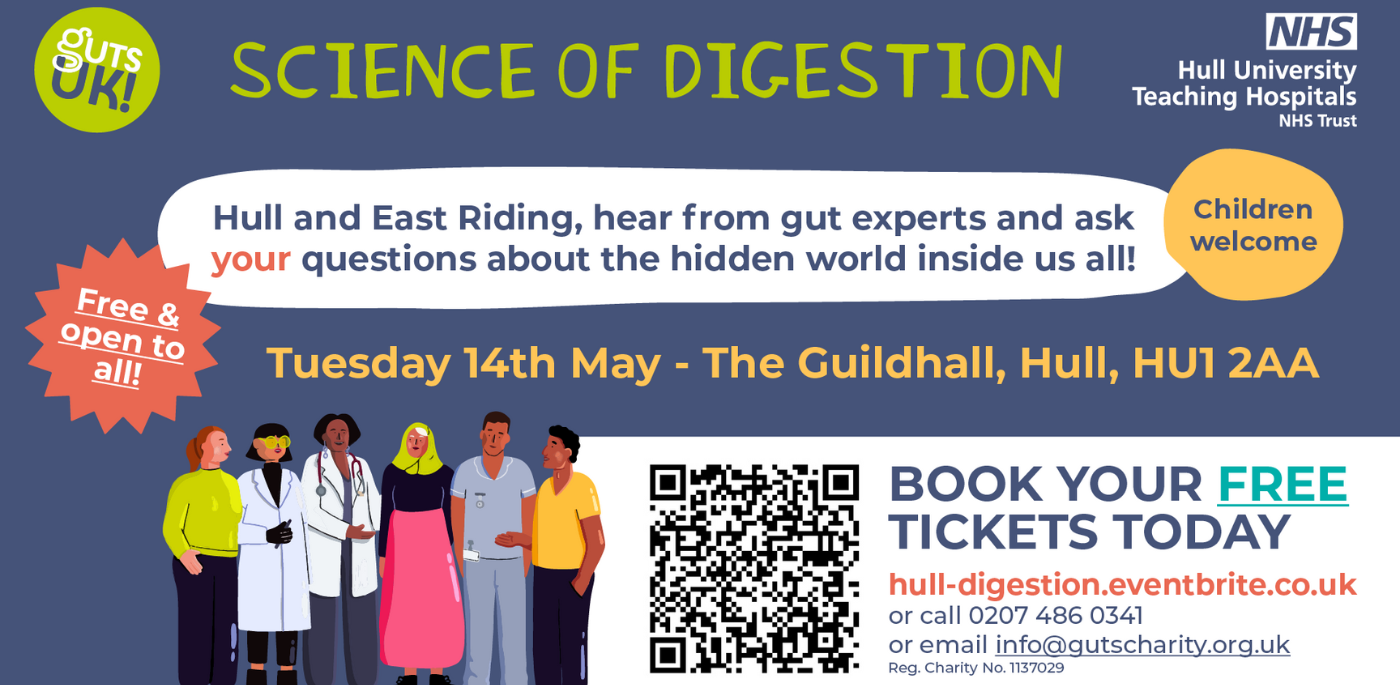

 “When it comes to gut health, as a nation we can’t afford to be embarrassed. Some 10,000 people are dying in the UK from liver disease each year, bowel cancer is the fourth most common cancer and half a million people are already living with IBD. These are not small numbers, so the likelihood is that, even if you’re not affected personally, you’ll know someone who is.
“When it comes to gut health, as a nation we can’t afford to be embarrassed. Some 10,000 people are dying in the UK from liver disease each year, bowel cancer is the fourth most common cancer and half a million people are already living with IBD. These are not small numbers, so the likelihood is that, even if you’re not affected personally, you’ll know someone who is.

