A marathon runner who suffered a cardiac arrest after a yoga class has run 10k alongside a physiotherapist who helped him back to health.
Mike Aramayo, 53, had a heart attack in Hull City Centre and was rushed to the specialist cardiology centre at Castle Hill Hospital.
However, he went into cardiac arrest and had to be resuscitated before he was taken into the operating theatre to have life-saving surgery.
Now, Mike has praised the Cardiac Rehabilitation Team after the team of physiotherapists helped him achieve his dream of running 10k within four months.
He said: “The whole team are absolutely amazing people and I cannot thank them enough.
“They gave me the courage to think I could get back to normal.
“They were always so positive, telling me I could have my life back again, and I don’t think I could have done this without their support.”
Mike, a managing director at a manufacturing firm in Burnley employing 800 people, lives in Hull with wife Joanne and they have three children – actress daughter Laura, 27, son Robert, 25, who has appeared in Game of Thrones and is currently in Hollywood filming and 20-year-old Charleigh, who is studying criminology.
A keen sportsman, Mike ran the London Marathon in 2016, completed the Great North Run and numerous 10k races. He also played football and squash.
He attended a yoga session every week and had just finished a class on May 3 when he became unwell.
“I was sitting in the changing room and this overwhelming tiredness came on me,” Mike said. “I had a shower but it kept getting worse and worse.
“By the time I got to my car, I couldn’t lift my bag up and started sweating. I then felt this massive pain in my chest and I knew I was in trouble.”
He managed to dial 999 but couldn’t speak so a woman stopped to help him and stayed with him until the ambulance arrived. The woman also answered his phone to Robert, who had only arrived back in Hull from New York the night before, and told him about his dad.
Robert arrived in time to accompany Mike to Castle Hill, alerting his mother and two sisters on the way, before they arrived at the hospital where Mike went into cardiac arrest.
“I was given two shots of morphine for the pain in the ambulance and don’t remember much,” Mike said. “I just remember brilliant white lights, then everything going dark, and then everything lighting up again.”
Mike was saved by the centre’s life-saving team before he went into theatre to have two stents fitted to keep his arteries open.
He spent three days in Intensive Care and a further night on a ward before he was allowed home, his heart back working at 90 per cent of its original capacity because of his baseline fitness.
He started a 16-visit programme over eight weeks, working with the Cardiac Rehabilitation Team at Hull Royal Infirmary.
“I told them my aim as soon as I went in there,” he said. “They knew how fit I’d been and I said my biggest goal was to run a 10k.
“And I did it on my very last session, with Oliver Sherwood, one of the physios, running on the treadmill alongside me.”
Despite his speedy return to health, Mike says the psychological barrier of having a heart attack was his toughest battle.
He said: “The psychological impact of having a heart attack is one of the biggest things you need to address.
“I think there are lots of people who have heart attacks and don’t believe it’s possible to get back to normal.
“Don’t get me wrong, I was very cautious at first and did everything they told me to do. I walked, cycled and I changed my diet, losing a stone even ‘though I wasn’t overweight before and no-one could give me a reason why I had a heart attack.
“I’ve taken these positive steps and I would love to be the person who goes in front of other people who have had heart attacks and says you can do it too.”
Oliver Sherwood, who ran the 10k with Mike, said: “Mike did absolutely brilliantly and he was fully committed to his rehab.
“He has achieved a huge goal of running 10k sixteen weeks after suffering a cardiac arrest. It really shows that our colleagues in the theatres at CHH do an amazing job.
“The whole of the Cardiac Rehabilitation Team are happy that we have been able to support and encourage Mike and our other patients in their journey.
“It’s hugely satisfying that we are able to make a difference to people following a cardiac event, be it running a 10k, playing with the grandkids or just feeling that life isn’t over following a heart attack.”





 Who are Allied Health Professionals?
Who are Allied Health Professionals?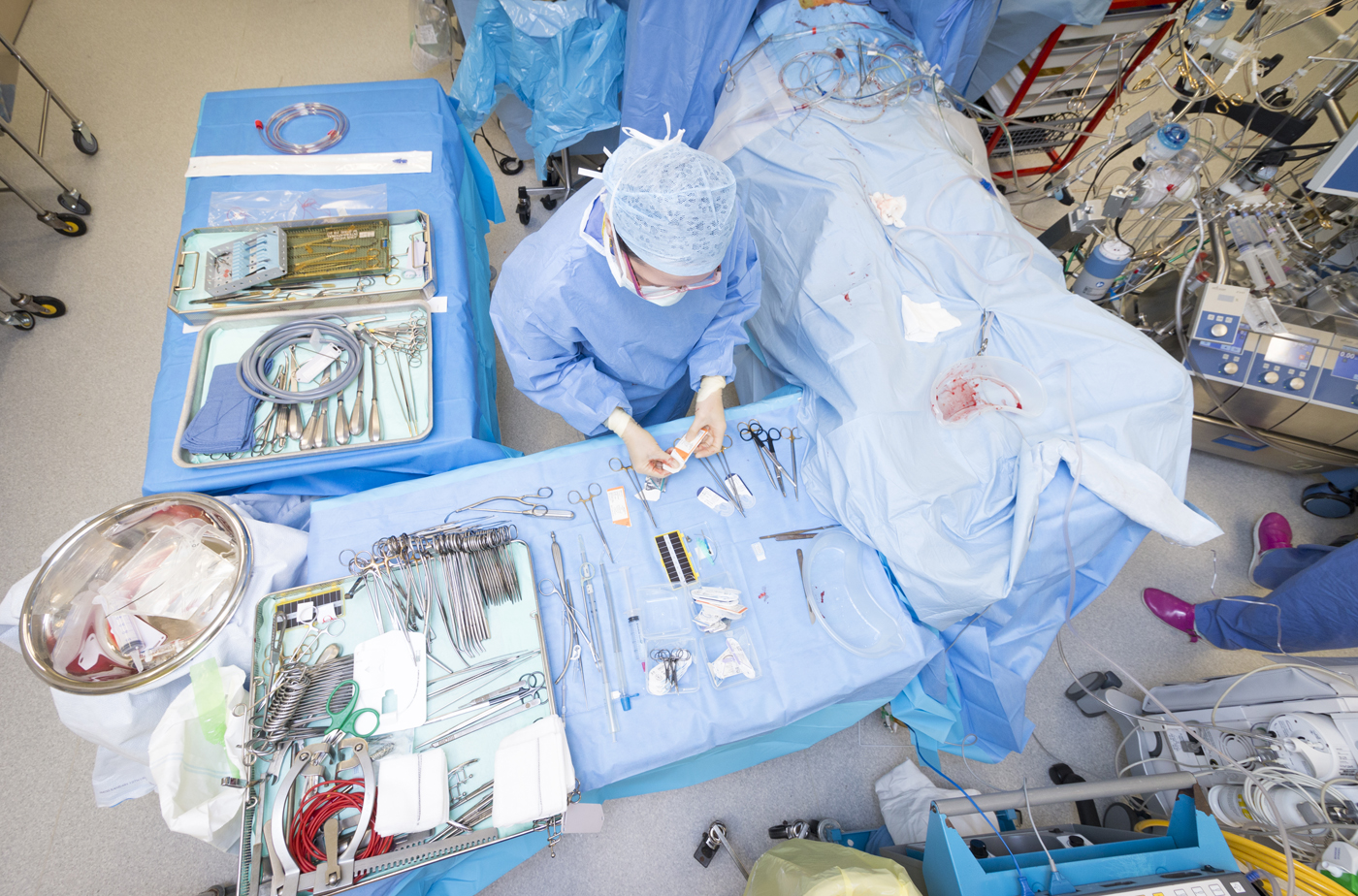
 Podiatrists
Podiatrists





 SIDS claims the lives of around 240 babies in the UK, with five dying every week.
SIDS claims the lives of around 240 babies in the UK, with five dying every week.

