Visitors are being urged to stay away from hospital when they are poorly as staff at Hull Royal Infirmary deal with this winter’s first outbreak of Norovirus.
Hull University Teaching Hospitals NHS Trust is asking visitors to stay away from Hull Royal Infirmary and Castle Hill Hospital if they have respiratory infections or sickness and diarrhoea as Ward 70 remains closed with the winter vomiting bug Norovirus.
Visitors should not come to hospital for at least 48 hours after symptoms of diarrhoea and sickness have stopped and only when they feel well enough following a respiratory infection.

Hospitals are particularly vulnerable to Norovirus, which spreads quickly in closed environments and among people with weakened immune systems, especially when patients or staff have symptoms which can be sudden in onset.
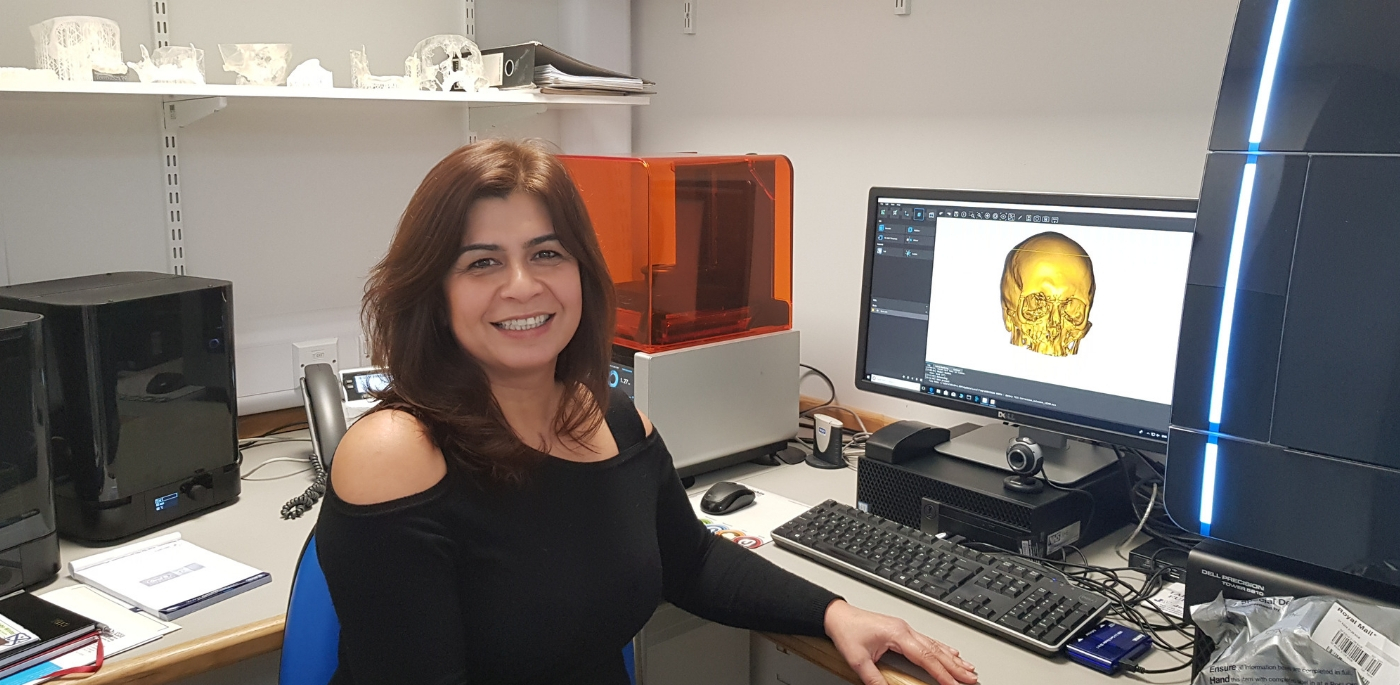
Greta Johnson, lead infection prevention and control nurse at the trust, said: “Our infection control team works really hard to control outbreaks when they happen and we have procedures in place to deal with the current outbreak.
“However, it would be a massive help if people could stay away when they’re ill instead of visiting relatives and friends in hospital.
“While you may want them to know you are thinking of them and want to see them, you don’t want to be responsible for making them more unwell by running the risk of passing what you’ve got onto them. You also don’t want to put yourself at risk of Norovirus as it’s an unpleasant illness to catch.”
The trust is appealing to people who do come to hospital to wash their hands as soon as they come onto wards, using the hand-washing facilities at the entrance as soon as they walk through the door. There are also hand-washing stations in the foyer of Hull Royal Infirmary next to the lifts.
Good hand hygiene, such as washing hands after using the toilet, is essential to prevent Norovirus and other infections spreading.
Covering your mouth when you cough or sneeze and disposing of paper tissues properly can also prevent the spread of respiratory infections passed through the air.
Norovirus can have a significant impact on hospitals, forcing the closure of bays and often entire wards at a time when beds are needed urgently to cope with an influx of patients over winter. Wards and bays can only reopen when they have had no new reported cases and patients have been symptom-free for 48 hours.