Parents-to-be are to be given a virtual tour of Hull Women and Children’s Hospital to explain the care they can expect before, during and after the birth of their babies.
Hull University Teaching Hospitals NHS Trust has produced a video providing an insight into maternity services provided by more than 280 midwives, midwifery assistants and clerical staff.
With around 5,000 babies born each year, the video takes viewers through the pregnancy journey from the moment women walk through the front entrance of the hospital.
Hull and East Yorkshire Women and Children’s Hospital from HEY Hospitals NHS Trust on Vimeo.
Janet Cairns, the trust’s Head of Midwifery, said: “Pregnant women and their birth partners were once able to come to hospital so they would be familiar with their surroundings when the time came for their babies to be born.
“However, these days, we can no longer offer that service to protect the dignity of the women using our service, to respect their privacy and to ensure good infection control procedures.
“But we appreciate there is still a need for women to be familiar with their surroundings and what they can expect.
“This video gives women a fantastic insight into the care they will receive from our amazing team throughout pregnancy, birth and after their babies are born.”
The video features the scanning department, where women find out when their babies are due, and the Antenatal Day Unit and Clinic, where midwives and doctors provide routine and urgent services for women before their babies are born.
It highlights the work of the community midwifery team, which supports women with antenatal and postnatal care and those choosing to give birth at home, and the antenatal and newborn screening teams, ensuring women are empowered to make the best choices for themselves and their babies.
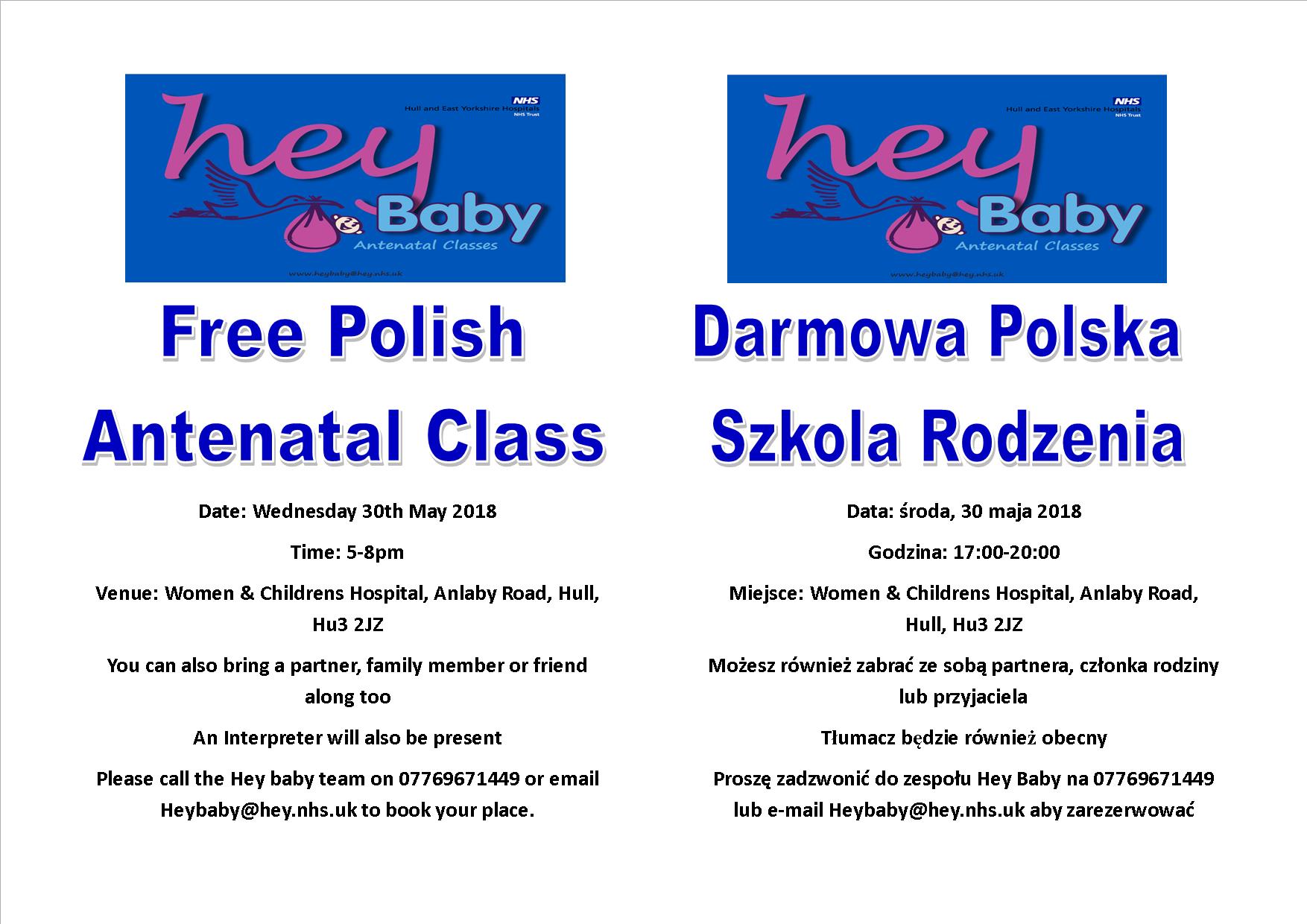
The work of the trust’s parent education service is showcased as the team supports antenatal classes and post natal classes across Hull and the East Riding. The HEY Baby Carousel, held on the last Wednesday of every month, has also been filmed with staff providing practical demonstrations of bathing, changing and helping babies to fall asleep safely.
The video, filmed by trust communications officer Chris Turner, also shows Maple Ward, the antenatal inpatient ward for women requiring more specialised inpatient care and where women can recover after their babies are born by caesarean section.
The Labour Ward, with teams of midwives, midwifery assistants and medical staff providing specialist care during labour and birth, also features in the video, with a pregnant woman filmed resting against a birthing pool in one of the ensuite labour rooms.
Viewers also get a virtual tour of the Fatima Allam Birth Centre, the midwifery-led unit where women with healthy pregnancies can have their babies in surroundings likened to a home from home environment rather than a hospital.
Specialist staff working in the obstetrics theatres helping women who need extra care and where babies are born by caesarean section are also shown during the seven-minute film.
The Neonatal Intensive Care Unit, looking after the sickest babies in the region, is also part of the video to show how the trust is able to care for those infants most in need of medical attention after birth.
Filming also took place on Rowan Ward, where women are taken after they have their babies in either a two-bed or single ensuite rooms.
The trust’s healthy lifestyle midwife, hearing screening team and infant feeding co-ordinators are also introduced to the public as well as the specially trained staff helping women with their emotional wellbeing at any stage of their journey to becoming a mum.
Midwife Melanie Lee, who leads the parent education team, said: “This is a fantastic video which shows women what wonderful services we have available.
“We hope it will help reduce anxiety and prepare them by showing them what is inside the doors of our amazing hospital.
“From our antenatal services right through to birth, whether that’s in the labour ward or the Fatima Allam Birth Centre, our staff are here to help parents throughout pregnancies and in those first few days after having their babies.”