- Reference Number: HEY288/2023
- Departments: Plastic Surgery
- Last Updated: 31 January 2023
Introduction
This leaflet has been produced to give you general information about what to expect following your surgery. Most of your questions should have been answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is Carpal Tunnel Decompression?
Carpal tunnel decompression is an operation to divide the tight ligament that compresses the median nerve as it enters the hand. Its aim is to reduce the symptoms of pain, tingling and numbness. You will have been given a leaflet entitled ‘Carpal Tunnel Syndrome: Your Diagnosis and Treatment Options’ which explains this surgery in greater detail.
What To Expect Following Your Operation
After your surgery your hand will be in a bulky dressing. We would encourage you to move your thumb and fingers as much as is comfortable. Some degree of discomfort is common but regular paracetamol and ibuprofen are usually excellent painkillers. The discomfort usually settles over a few weeks but occasional stabbing pain, scar pain and aching discomfort when gripping objects may persist for 3-4 months. Elevating your hand for the first few days is likely to help keep any swelling and pain to a minimum.
How To Manage Your Dressings
Please remove the bandage from your hand 2-3 days after your surgery. There will be a small adhesive plaster covering the wound which can be left in place for up to 10 days. Do not worry if the dressing peels away earlier, it does not need replacing. Please keep your wound clean and dry for at least 48 hours. Try and massage your scar with simple moisturising cream twice daily for at least 6 weeks, starting as soon as possible after your operation.
Complication and Signs to Look Out For
Infection – redness, increasing pain, wound discharge
Bleeding – excessive bleeding from the wound (a little dried blood on the dressing is normal)
Stiffness – your hand should be moving ‘normally’ within 2 weeks
Pain – any severe or increasing discomfort
Follow Up Plan
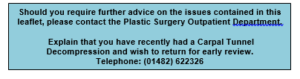
We do not routinely need to bring you back to the outpatient clinic following your surgery. Following discussion with you we will arrange either a Patient Initiated Follow Up (this enables you to contact us in the three months after the operation if you have any concerns and would like to be seen), or an appointment to see you in the outpatient clinic 6-8 weeks after surgery particularly if you have similar problems affecting the other hand. If you have any concerns or problems before then please contact us as detailed below:
This leaflet was produced by the Plastic Surgery Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in January 2026.
Ref: HEY288/2023
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

