- Reference Number: HEY1370/2023
- Departments: Paediatrics, Physiotherapy, Therapies
- Last Updated: 31 August 2023
Introduction
This leaflet has been produced to give you general information. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a Patient-Initiated Follow-Up (PIFU) pathway?
A patient-initiated follow-up (PIFU) means that we will not routinely book you an appointment, instead we are putting you in control of making your own appointments at a time when you need them most, within a given timeframe.
How does PIFU work?
You will have been given this leaflet because your healthcare professional is happy that you do not need to see them again unless you have a problem. If you do have any problems, you can contact the Paediatric Therapy department on the given telephone number and they will arrange an appointment, either by telephone or face-to-face if it is needed. You will be told how long after your injury that you can contact the Paediatric Therapy department, on the PIFU pathway if you need to be seen.
When should I call for a PIFU?
You can call to make an appointment if you
- are not improving to a level that was expected
- have worsening symptoms relating to your injury/condition
- have a “flare-up”
Please note, you can only initiate a PIFU appointment for the specific injury/condition you were originally referred to the Paediatric Therapy service for.
When should I not use PIFU?
- If your concern is related to different injury/condition
- If the specified time period has lapsed, please contact your GP.
- If you need urgent medical advice you should contact your GP or NHS111.
What if I don’t need a PIFU follow-up appointment?
You do not have to arrange an appointment if you feel it is not required. If you don’t contact us to book an appointment within the specified timeframe, the PIFU will expire and you will be discharged back to the care of your GP. We will not contact you to book a PIFU appointment – it must be initiated by you.
What is a Phalangeal Fracture?
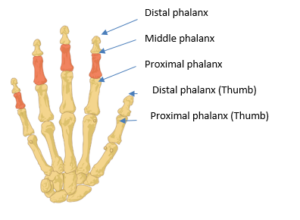
A phalangeal fracture is a break of a phalanx (one bone) or phalanges (more than one bone) in your finger or thumb.
Each finger has 3 phalanges. Proximal (nearest your palm), middle and distal (at your finger tip). The thumb has only 2, a proximal and distal phalanx.
Your fracture can be described as simple, stable or un-displaced. This means there is likely to be a clean break, but the pieces of bone are in the correct position, and are unlikely to move out of place.
How should it be treated?
The broken bone will heal in about 3 weeks. During this time it is necessary to protect it from excessive stress.
The finger or thumb is likely to be placed in a splint. Occasionally the finger may be taped to the one next to it this is called buddy or neighbour strapping.
What should I do in the first few days?
It is normal for the hand to be painful and swollen following this injury, sometimes even spreading to parts of the hand that were not injured. However, although a normal reaction, swelling which stays in the fingers and thumb too long, becomes very dense and sticky (fibrous) and can result in long term stiffness. To prevent this we advise that you:
- Allow your hand to rest slightly for the first 48 hours
- Take over the counter pain relief such as paracetamol
- Keep your hand elevated above your heart
- Move all of the uninjured fingers fully and often
- Use your hand as normally as possible, as your comfort allows, for everyday daily tasks such as dressing and eating meals.
You will have been told how long to wear the cast, splint or strapping for, after which time you can remove it yourself. No further X-ray will be needed.
Exercises
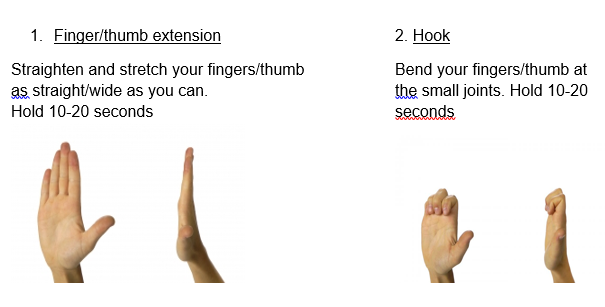
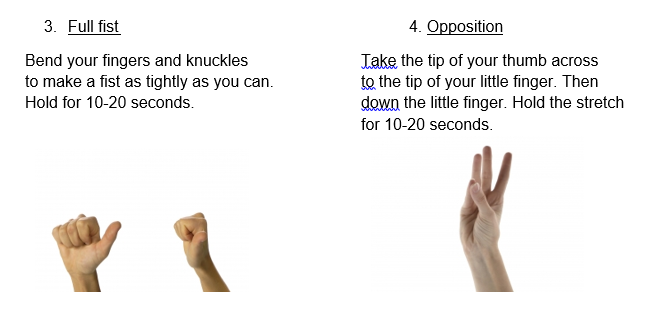
Soft tissues such as tendons and ligaments, need to keep moving as the fracture heals otherwise they will become stuck leading to long term stiffness and discomfort. It is therefore important to begin exercising the injured finger or thumb regularly, once the splint is removed. Buddy strapping can remain in place during the exercises.
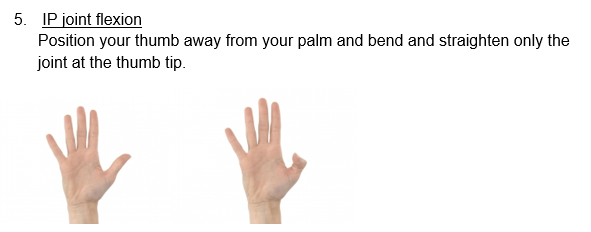
The following exercises should each be repeated 10 times and completed every 2-3 hours. Support your elbow on the table with your wrist straight.
What about play and school?
You can use your hand for light daily activities such as eating, dressing and light school activities as soon as you feel comfortable. Carrying heavy bags or attending PE at school is best avoided until 6 weeks after your injury.
Full contact sport should also be avoided for at least 6 weeks and until you have full range of movement and strength. You should start by practicing sports specific activities; like throwing or catching. Build up these activities gradually from around 6 weeks in order to regain strength and flexibility before returning to full training sessions and competition.
When should I call for a Patient Initiated Follow Up (PIFU) appointment?
It may take several months for discomfort to settle, and the finger or thumb may appear ‘thicker’ than on your other hand. This is normal.
You should initiate a PIFU appointment if:
- You have any problems with the splint (if you have one)
- If pain and swelling isn’t starting to settle within 3 weeks, or is getting significantly worse
- If you notice the position of the finger or thumb appears to have changed, such as being at an angle or rotated.
Or if after 3 weeks of exercise you are unable to:
- Fully straighten your finger or thumb.
- Make a fist, or get your fingertip to your palm.
- Touch the tip of each finger, and reach the base of your little finger with your thumb.
- You are struggling with light daily tasks
Or after 6 weeks, you are struggling to return to your daily activities or hobbies.
If we do not hear from you 3 months following your injury date we will assume that you no longer require any further intervention and will be discharged from the PIFU pathway. If you have further problems with your finger after this date please contact your GP practice
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Paediatric Therapy Department on telephone: 01482 674539.
This leaflet was produced by the Paediatric Therapy team, Hull University Teaching Hospitals NHS Trust and will be reviewed in August 2026
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats your child, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to your child. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your child’s condition, the alternatives available for your child, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about your child
We collect and use your child’s information to provide your child with care and treatment. As part of your child’s care, information about your child will be shared between members of a healthcare team, some of whom you may not meet. Your child’s information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide your child with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your child’s doctor, or the person caring for your child.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about your child. For further information visit the following page: Confidential Information about You.
If you need information about your child’s (or a child you care for) health and wellbeing and their care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

