- Reference Number: HEY1373/2023
- Departments: Gynaecology, Oncology (Cancer Services)
- Last Updated: 31 July 2023
Introduction
This leaflet has been produced to give you general information. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
This leaflet explains what will happen now that you have had your postoperative follow up appointment after your surgery to treat your cancer.
What is a patient initiated follow up (PIFU)?
Now you have completed your treatment, you and your cancer team need to discuss your routine follow up appointments.
Most patients with a low-risk cancer that has been fully treated do not require regular follow up appointments by the hospital team. Attending regular outpatient appointments scheduled by the hospital can cause unnecessary anxiety, for instance waiting for your appointment to come through and time taken to travel and find a parking space.
Instead, some patients can be offered patient initiated followed up (PIFU for short). This allows you to arrange follow up appointments when you need them, for instance if your symptoms flare up or your circumstances change.
PIFU puts you in control of your hospital follow up and enables us to create capacity to see a consultant when and if you need to.
This will be discussed with you at your follow up appointment following surgery by the consultant or by the Clinical Nurse Specialist team.
Can there be any complications or risks?
Research has shown that the PIFU approach to care is not detrimental to your clinical care. Regular outpatient appointments may not result in a change to your treatment. In fact, symptoms may arise in between regular booked appointments and it’s during this time you really need our input. You will be on PIFU for 2 years following surgery. You can contact the Clinical Nurse Specialist team during this time and then we can discuss symptoms or concerns and make you an appointment if necessary. You will be given advice sheets and contact details to ring if you have any concerns or symptoms that require an appointment.
Who do I call if I have any concerns or questions?
You will be supported by the Gynaecology oncology Nurse Specialist team for 2 years following surgery. You can contact the team throughout this period if you have any concerns relating to your cancer treatment on Telephone number 01482 624033
When should I call?
You should telephone us if
- You have symptoms that you are worried about, causing you to think that your cancer has returned
- You have ongoing problems or side effects after your treatment
- You need emotional support
What Symptoms should I call for advice about?
If you have any of the following symptoms for no apparent reason that last longer than a few days
- Bleeding from your vagina
- Vaginal discharge
- Bleeding from your back passage
- Bleeding after sexual intercourse
- Pelvic pain
- Problems passing urine
- Diarrhoea or constipation
- Abdominal bloating that does not go away
- Swollen legs or pain in the back of your legs
- Weight loss (non- intentional)
- Feeling generally unwell
- Persistent dry cough
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Gynae-Oncology Clinical Nurse Specialists on: 01482 624033
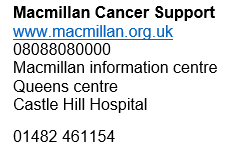
Other support available
This leaflet was produced by the Gynaecology oncology Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in July 2026
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

