- Reference Number: HEY1434/2024
- Departments: Dietetics, Nutrition Support
- Last Updated: 29 February 2024
Introduction
This leaflet is for anyone who has been advised that they need to follow a low phosphate diet.
What is phosphate?
Phosphate is a mineral found in many foods and drinks. It helps to build healthy bones and teeth. Healthy kidneys usually filter and get rid of excess phosphate from the blood and help to keep the phosphate levels at the correct level. If your kidneys are not working properly, phosphate can build up in your blood.
Why does it matter if my phosphate level is too high?
High blood phosphate levels in the short term may cause:
- Red eyes and itchy skin
Continued high phosphate levels can eventually lead to:
- Weaker bones and aching joints
- A build-up of calcium deposits leading to hardened blood vessels, increasing your risk of heart disease.
What can I do to help reduce my phosphate levels?
Dietary advice can help to reduce your phosphate intake, this should be given by a renal dietitian and will take into account other dietary requirements you may have.
- Step 1 is to reduce your intake of phosphate additives
- Step 2 is to reduce your intake of high phosphate foods and drinks
- Step 3 is to take phosphate binders
Your diet and phosphate binders may need to change over time, depending on your appetite and any other medications and treatment for your kidneys.
How to achieve a low phosphate diet
Step 1: Reduce your intake of Phosphate additives
Phosphate additives are used during the food manufacturing process. They help to keep food moist, improve taste and texture, or extend the shelf life. Approximately 50% of the phosphate we eat comes from these additives and they are easily absorbed by the body.
By checking the labels of any processed or packaged foods you can see if they contain any phosphate additives. Different brands of the same foods will contain phosphate additives and others none so you will need to just read the label.
Below is a list of phosphate additives to look for on ingredients list. The phosphate additive will be listed either by its full name or by its E number. Look out for ‘phos’!
| E number | Name of Additive |
| E338 | Phosphoric acid |
| E339 | Sodium phosphates |
| E340 | Potassium phosphates |
| E341 | Calcium phosphates |
| E343 | Magnesium phosphates |
| E450 | Diphosphates |
| E451 | Triphosphates |
| E452 | Polyphosphates |
| E541 | Sodium aluminium phosphates |
Step 2: Reduce your intake of high phosphate foods
The following list foods that are high in phosphate and gives lower phosphate alternatives. We have also indicated which of these foods may contain phosphate additives but this can vary according to manufacturer which is why it is important to check the ingredients list. If there are any foods or drinks that are not included you can ask your dietitian for advice.
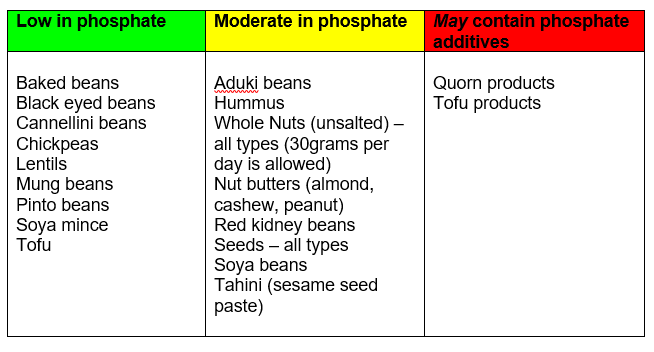
Meat, Fish and Eggs
These foods are good sources of protein, which is important for your overall health and wellbeing as well as building and maintaining muscle and for fighting infection.
Ensure you have these foods, or vegetarian and vegan alternatives, with at least two meals each day to ensure you have enough protein in your diet.
Use the following table to make suitable choices.
Check that your serving sizes are similar to those suggested.
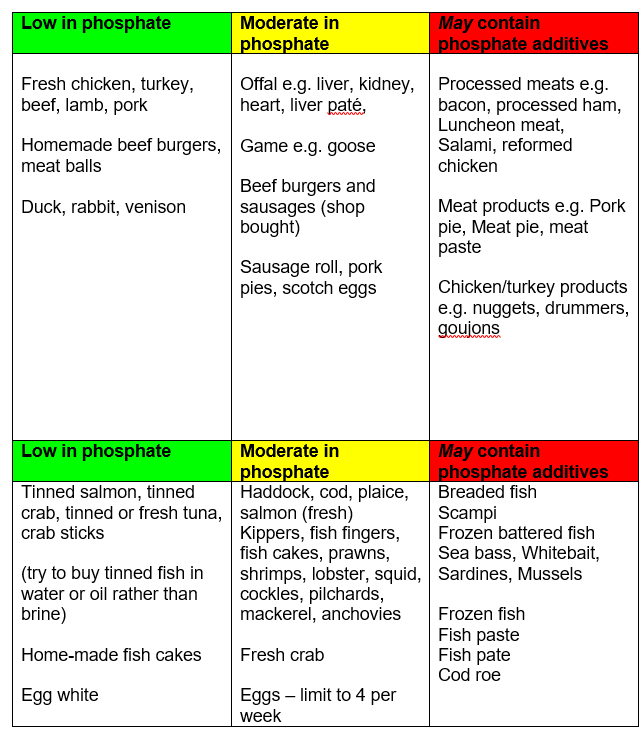
Suggested Serving Sizes:
Light meal:
- 1 to 2 slices cold meat: 30 to 60 grams (1 to 2 ounces)
- tinned tuna/salmon/mackerel 30 to 60 grams (1 to 2 ounces)
- 1 to 2 eggs
Main meal: 90 to 120 grams (3 to 4 ounces) cooked weight (about the size of the palm of your hand)
- 3 slices roast meat/1 average sized chop
- 1 chicken breast or Quorn fillet
- 1 fillet of fish
- 2 vegetarian sausages
- 4 tablespoons of chickpeas
- 2 to 3 eggs
- 3 tablespoons of cooked beans/pulses
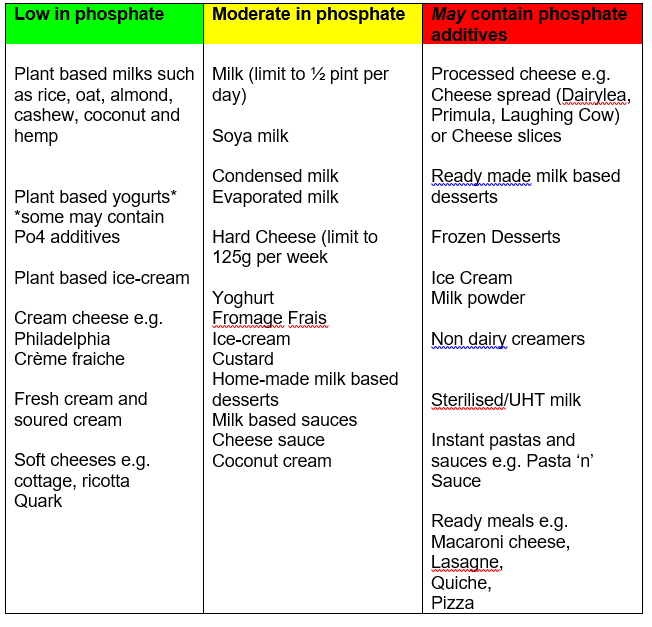
Milk and Dairy foods
Dairy foods such as milk, cheese and yoghurt are important sources of protein, vitamins and minerals. However, they are higher in phosphate than other high protein foods such as meat and fish, so it is important not to have too much.
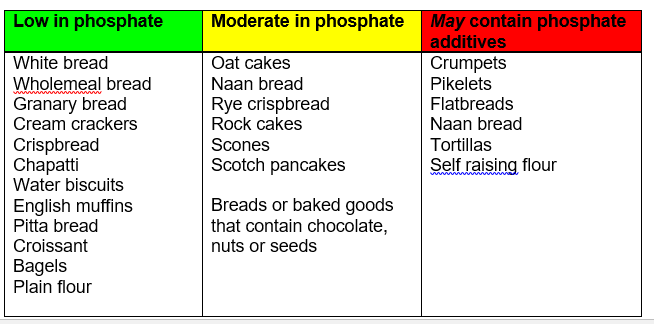
Bread, Rice, Potatoes, Pasta & other starchy foods
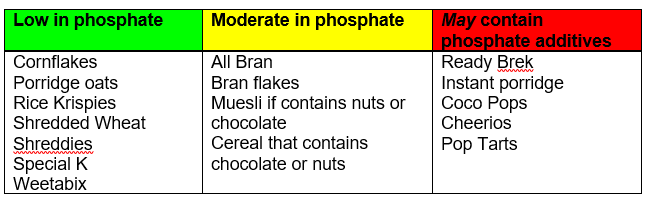
Breakfast Cereals
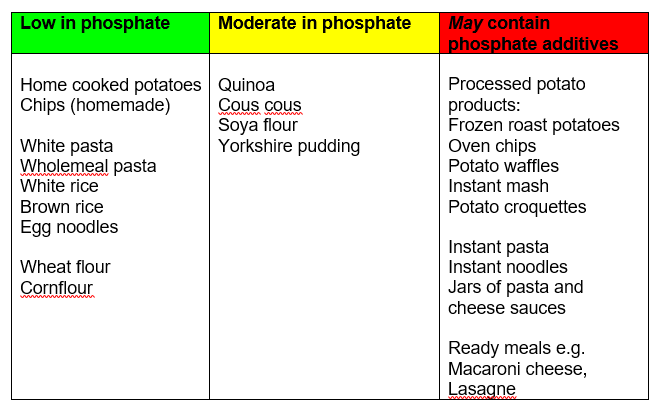
Rice, Potatoes, Pasta and Grains
Tips to reduce phosphate:
- Make porridge with half milk or cream/half water.
- Swap to dairy free milks to have with cereal.
- Try to make your own white and cheese sauces.
- Ideally make your own mash, roast and chipped potatoes and use frozen potato products sparingly.
Foods High in Fat and/or Sugar
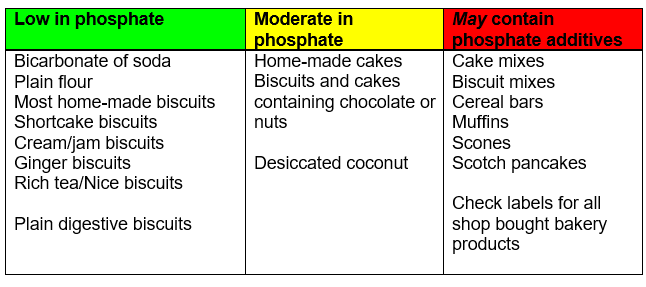
Many baked goods contain phosphate, the main sources being baking powder or self-raising flour. Processed foods such as cake mixes often have a higher phosphate content than the equivalent home cooked variety.
Fats and Oils
Most fats/oils are low in phosphate. Those marked ♥ are better for your heart.
| Monounsaturated fats ♥ | Olive oil, rapeseed oil, olive oil based spreads |
| Polyunsaturated fats ♥ | Sunflower, soya, corn oils and margarines made from these oils |
| Saturated fats | Butter, cream, lard and visible fat on meat, coconut oil |
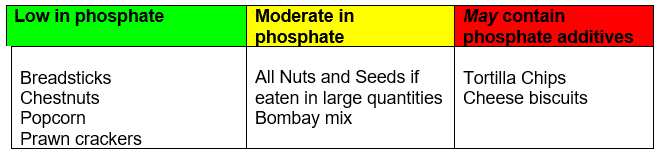
Savoury Snacks
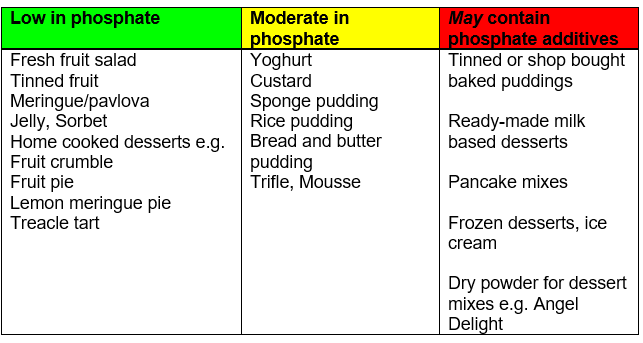
Puddings
Tip!
Extra snacks between meals and puddings may be useful for those with a poor appetite who are only managing small meals.
Serve puddings with cream or crème fraiche instead of custard or ice cream.
When making cakes at home, try to avoid the use of baking powder.
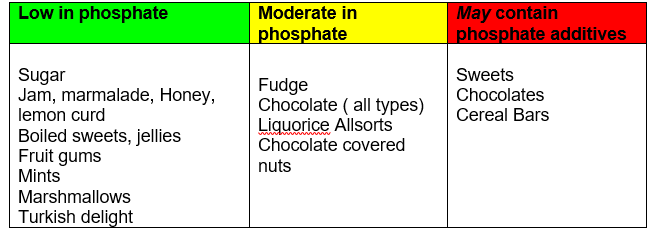
Sugar and confectionary
Biscuits and cakes
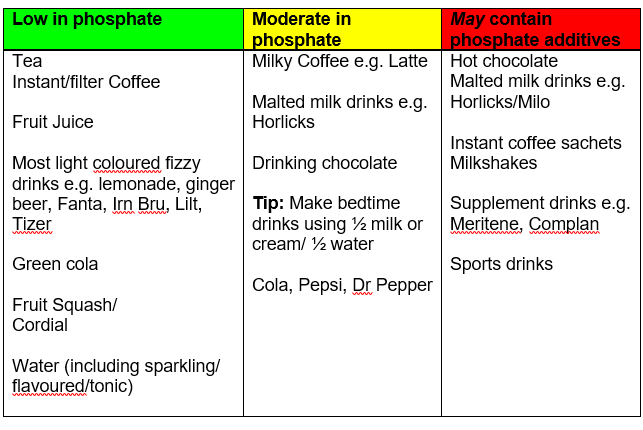
Drinks
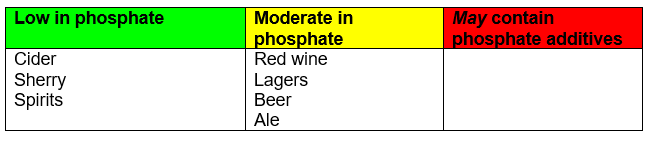
Alcohol
Miscellaneous
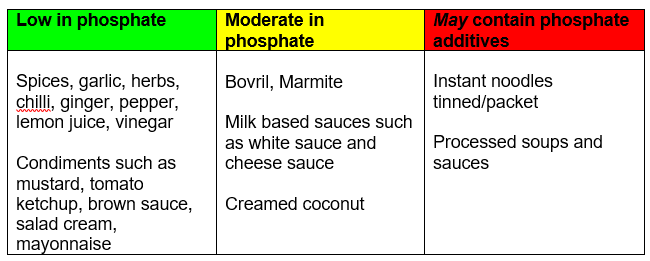
Tip!
Try to make your own sauces and soups rather than using pre-prepared jars, packets or tins as you will not add any additional phosphate additives.
Step 3: Phosphate Binders
Why might I need phosphate binders?
In addition to a low phosphate diet you may be prescribed some medication called phosphate binders. Binders combine with some of the phosphate in your food when it is being digested in your stomach, allowing it to pass out of your body with your stool (poo).
To work properly you need to take your binders with all meals and snacks as discussed with your dietitian.
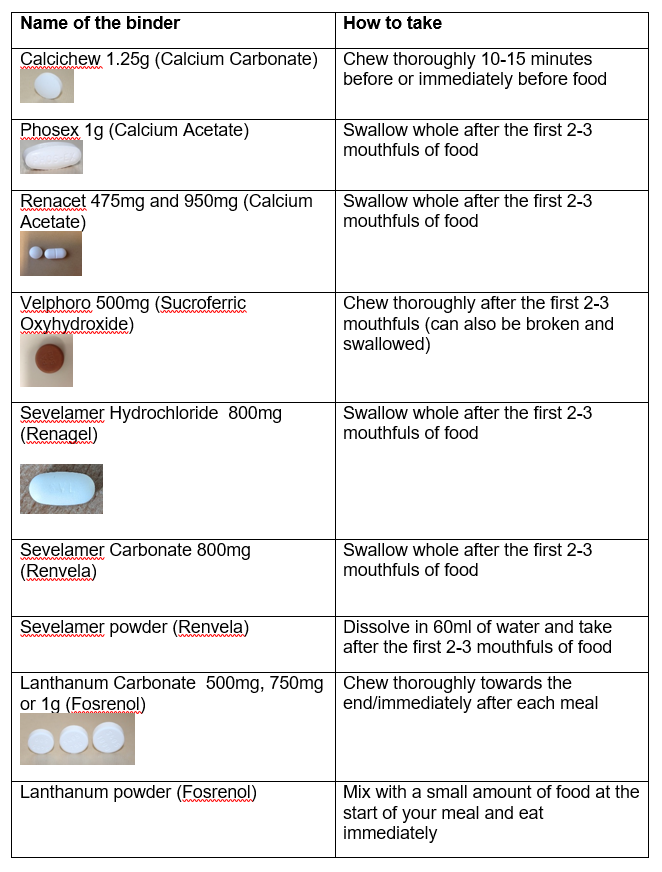
What if I forget to take my phosphate binder?
Timing is everything: Be sure to take your binders when you eat food — the longer you wait, the less they work. If you have a meal or substantial snack on dialysis you will need to take your binders with this.
To help you remember your phosphate binders try setting an alarm on your mobile phone to go off around meal times. Keep a small pot of phosphate binders in your bag or pocket to take when you are out. You can also put a small pot of binders in your cutlery drawer or where you eat your meals.
If you take insulin put you binders alongside to remind you to take them with your meals.
A very small number of people may find that they have side effects from their phosphate binders. If this is the case for you, please speak to your renal dietitian or nurse.
Further information
For more information on following a low phosphate diet you can watch this useful webinar:
https://patientwebinars.co.uk/condition/kidney-health/webinars/
For more information please contact the renal dietitians on tel: 01482 674707, please leave a message and we will return your call as soon as possible.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

