- Reference Number: HEY1441/2024
- Departments:
- Last Updated: 30 April 2024
Introduction
This leaflet is to provide you with information about a total laparoscopic hysterectomy which is removal of womb through a keyhole surgery.
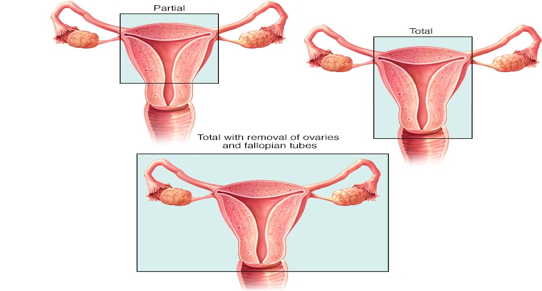
There are several different types of hysterectomy, including:
- Total hysterectomy is where both the uterus and cervix (neck of the womb) are removed
- Subtotal hysterectomy is where just the uterus is removed and the cervix is left behind.
- Hysterectomy with salpingo-oophorectomy (removal of one or both of your ovaries and your fallopian tubes) at the same time. This depends on your age, and the cause for hysterectomy. This will be discussed with you by your doctor before the surgery. We may also remove pelvic lymph nodes if your surgery is to treat a cancer.
- Total laparoscopic hysterectomies are done entirely by keyhole surgery.
- Some are done partially through your vagina (sometimes called a laparoscopic assisted vaginal hysterectomy or LAVH)
Why do I need a hysterectomy?
There are many reasons why a woman may need a hysterectomy which include; heavy or painful periods, fibroids, pelvic pain, prolapse or a gynaecological cancer. Your doctor will discuss this with you.
What are the benefits of a keyhole operation?
There are several advantages to having a hysterectomy by the laparoscopic or keyhole approach. These include less scarring, less pain after the operation, a shorter stay in hospital and a quicker return to normal life.
How do I prepare for surgery?
Before surgery you will be seen in a pre-assessment appointment for blood tests, medications check (if you are on any). You may have an ECG or investigations relevant to your health conditions. On some occasion you may be seen by the anaesthetic doctor before surgery.
Common problems could be eg: low iron level, high blood pressure or poorly controlled diabetes which will need optimisation before surgery which could be done by your GP in liaison with your gynaecologist.
Day of surgery
On the day of operation you will be seen by gynaecology doctors, nurses and anaesthetic doctor and be prepared for the surgery
What happens during surgery?
A TLH is carried out under a general anaesthetic (being put to sleep).
A narrow plastic tube called a cannula is inserted into a vein in your arm or hand using a needle; this is used to give you fluids and medications.
After you have been given a general anaesthetic and you are asleep, a catheter (a tube for urine drainage) is inserted into your bladder.
A small cut of 1 to 2 cm (centimeters) is made in or around belly button – this is used to put gas in your abdomen and also to insert camera. Some additional cuts on either side of tummy wall and cut in your lower tummy of around 1 cm (centimeter) is made. These cuts are for other instruments to be inserted to perform the surgery.
Your ovaries and fallopian tubes may or may not be removed depending on the reason for your surgery. The uterus, cervix and tubes, ovaries are removed through vagina in almost all cases. If uterus is too large to be removed vaginally, or the vagina is too narrow, on very rare occasions another cut might have to be made on abdomen to take it out.
Overall the surgery takes 2 to 3 hours and approximately 4 to 5 hours including anaesthesia and recovery.
Are there any risks of complication with this surgery?
Common problems after surgery include pain, infection, vaginal bleeding, feeling bloated or having shoulder tip pain due to trapped wind and urinary tract infection.
Complications such as injuries to bladder, bowels, ureters (tubes connecting kidney and bladder) are uncommon and injury to major blood vessels are rare. Blood transfusion may be needed on occasions if excess blood loss occurs.
Because of prolonged hours of surgery and reduced mobility after procedure there is a significant risk of developing blood clots in the leg or chest. Preventative measures are taken for few days to weeks depending on your background health risks.
After surgery
You will have some dressing on your skin stitches, and a catheter draining urine and on some occasions a dressing pack in the vagina.
Your skin stitches are all dissolvable and so are the sutures in vagina. The dressings on skin stitches can be removed on day 1 after the surgery and start using the antibiotic cream given.
Day 1
The catheter is removed and pack (if present) will be removed at the same time. You will be encouraged to eat and drink, mobilise and ensured you are on the recovery pathway. On some occasions you may need a blood test to check your iron levels.
If you have managed to mobilise, pass urine on your own and remained well you will be discharged home. On an occasion you may need to stay until day 2 or 3 until you are well enough to be discharge home. Your doctor will discuss this with you.
Recovering at home
You can expect some vaginal bleeding up to a week or two after operation. This is light brown to red, light bleeding. You should use sanitary towels and avoid using tampons as these increases risk of infection. You should seek medical attention if bleeding is heavy, notice offensive odour, develop fever or feeling unwell. You should contact your local GP.
You can expect pain and discomfort in your lower abdomen for at least the first few days after your operation. You may also have some pain in your shoulder. This is a common side effect of laparoscopic surgery. When leaving hospital, you should be provided with painkillers for the pain you are experiencing. Sometimes painkillers that contain codeine or dihydrocodeine can make you sleepy, slightly sick or constipated. If you do need to take these medications, try to eat extra fruit and fibre to reduce the chances of becoming constipated and can also use laxatives to help avoid constipation.
Reducing risk of blood clots
You can reduce risk of blood clot formation by keeping yourself as much mobile as possible.
- Have a gentle walks inside the house.
- Pump each foot up and down briskly for 30 seconds by moving your ankle and move each foot in a circular motion for 30 seconds.
- Bend and straighten your legs – one leg at a time, three times for each leg.
- Daily heparin injections (a blood thinning agent) will be started as soon as 6 hours after surgery and are to be continued at home. The duration of the injection would be at least 10 days or longer depending on the medical condition. It will be discussed with you by your doctor.
- You will also be given compression stockings to be worn at home, day and night, until you are mobilising reasonably well.
Returning to work
We advise you to take off work for 6 weeks at least. Depending on the type of job you may wish to take longer if your work entails manual lifting moving
Driving
You should be able to drive after 4-6 weeks and be able to safely carry out an emergency stop.
Starting HRT (hormone replacement therapy)
If your ovaries have been removed during your operation, you may be offered hormone replacement therapy (HRT). This will be discussed with you by your gynaecologist and together you can decide the best way forward. Most HRT treatments that are in the form of patches can be started 2 to 3 weeks after surgery whilst tablet forms are best avoided to up to 6 weeks after surgery.
Cervical screening
Some women who have had a laparoscopic hysterectomy will need to continue to have smears from the top of the vagina. This is communicated to you and your GP soon after we receive the report on your womb, cervix, tubes and ovaries. Check with your GP or gynaecologist as to what applies to you.
Tiredness and feeling emotional
You may feel much more tired than usual after your operation as your body is using a lot of energy to heal itself. You may need to take a nap during the day for the first few days. A hysterectomy can also be emotionally stressful and many women feel tearful and emotional at first – when you are tired, these feelings can seem worse. For many women this is the last symptom to improve.
The top of the vagina could have some stitches that can take up to 6 weeks to dissolve. You will need to allow healing time before resuming intercourse.
Recovery Tracker
1 to 2 days after operation
How might you feel?
- You are likely to be in hospital during this time.
- You will have some pain and discomfort in the abdomen.
- You may feel sore moving in and out of bed.
- You may have some bleeding like a light period.
What is safe to do?
- Get up and move about.
- Go to the toilet.
- Get yourself dressed.
- Start eating and drinking as usual.
- You may feel tired and perhaps feel like a sleep in the afternoon.
Fit to work
- No
3 to 7 days after operation
How you might feel?
- You will be at home by now.
- Your pains will slowly be reducing in intensity and you will be able to move about more comfortably.
- You will still tire easily.
What is safe to do?
- Continue as for days 1 to 2.
- Go for short walks.
- Continue with exercises that have been recommended to you.
- Wash and shower as normal.
- Have a sleep or rest in the afternoon if you need to.
Fit to work?
- No
1 to 2 weeks after operation
How might you feel?
- There will be less pain as you move about and you will find your energy levels slowly returning.
- Bleeding should have settled or by very little.
What is safe to do?
- Build up your activity slowly and steadily.
- You are encouraged to go for longer and more frequent walks.
- Restrict lifting to light loads.
Fit to work?
- Not just yet.
2 to 4 weeks after operation
How might I feel?
- There will be even less pain now as you move more and more.
- You will find your energy levels returning to normal.
- You should feel stronger every day.
What is safe to do?
- Continue to build up the amount of activity you are doing towards your normal levels.
- You can start to do low-impact sport.
- Make a plan for going back to work.
Fit to work?
- Yes – possibly on reduced hours or lighter duties at first. Some women will be fit for full-time work after 4 weeks.
4 to 6 weeks after operation
How might I feel?
- Almost back to normal.
- You may still feel tired and need to rest more than usual.
What is safe to do?
- All daily activities including lifting.
- Usual exercise.
- Driving.
- Have sex if you feel ready.
Fit to work?
Yes – but if you don’t feel ready to go to work, talk to your GP or employer about the reason for this.

