- Reference Number: HEY1414/2024
- Departments: Physiotherapy
- Last Updated: 29 February 2024
Introduction
This leaflet has been produced to give you general information about Achilles tendon rupture and its management. It is not intended to replace the discussion between you and the healthcare team but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
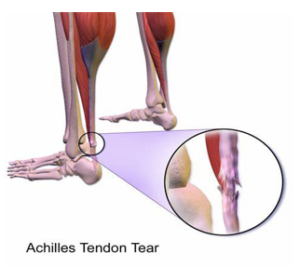
What is the Achilles tendon?
The Achilles tendon is a strong tendon which attaches your calf muscle to your heel. It functions to allow you to point the foot/ankle downwards, stand on tiptoes and to allow a good push off from your foot when you walk and run.
Achilles tendon rupture – Wikipedia
Injury to the Achilles tendon is commonly caused by a sudden increase in the load or stress placed on it. This can occur during activities that involve running and jumping. It can also be injured following a fall or misjudging a step. Occasionally, the Achilles tendon is weak due to pre-existing tendinopathy making it more prone to rupture with minor injuries.
Diagnosis
A health care professional will examine you in the minor injury unit or the emergency department and ask you about how the injury occurred.
Once an Achilles tendon rupture is suspected you will be placed in a below knee plaster cast with your foot pointing downwards.
A venous thromboembolism (VTE) assessment will be undertaken and quite often blood thinners will be prescribed for a 6 week duration. This minimises the risk of developing a clot (DVT).
To confirm an Achilles tendon rupture you will be referred for an ultrasound scan which should be undertaken within 2 weeks.
X-rays are not useful with this type of injury as there is no bone involvement.
Conservative management (Physiotherapy led)
Based on current evidence, most patients are treated under physiotherapy supervision without the need for surgery, allowing the tendon to heal naturally. Occasionally, you may be offered surgical repair. You will be seen by the physiotherapist approximately 2 weeks after your fracture clinic appointment.
Conservative treatment plan
| Weeks since injury | Plan |
| 0-2 weeks |
The ultrasound department will contact you to arrange an appointment for your scan |
| 2 weeks |
Continue in the walker boot at all times including night time (can be removed for hygiene purposes only) |
| 4 weeks |
Continue in the walker boot at all times including night time (can be removed for hygiene purposes only) |
| 6 weeks |
Continue in the walker boot at all times including night time (can be removed for hygiene purposes only) |
| 10 weeks |
If the tendon has healed, you will commence walking in your own shoes and commence some ankle exercises as instructed by your Physiotherapist |
| Week 10 onwards |
You will have a follow up appointment in Orthopaedic clinic 9-12 months post injury which your Physiotherapist will arrange |
Care while in the walker boot
You are encouraged to weight bear in the boot. Continue to take blood thinning injections/tablets for 6 weeks unless you have been told otherwise by your consultant. Your boot must be worn at all times, including in bed to enable the tendon to heal. However, it is important to clean your leg and check your skin to ensure there are no areas of redness, blistering or skin breakdown. You will be shown how to carefully remove/replace your walker boot and to change your sock. If you have any concerns about the skin condition, contact the physiotherapy department on 01482 608939 to inform your physiotherapist.
Surgical management
Surgical repair is occasionally indicated in young high demand athletes, particularly where there is a large gap between the tendon ends as shown by ultrasound scan. Surgical repair is also indicated in patients with delayed presentation. Surgical repair leads to good long-term outcomes but with an added risk of surgical complications. You will be immobilised in a boot or cast for the same amount of time as those treated without surgery. Your consultant will discuss this in more detail with you at your fracture clinic appointment.
Can I work following an Achilles tendon rupture?
This depends on what your job involves. Your physiotherapist will be able to advise you on this. If you require a FIT for work note your consultant in clinic or physiotherapist can provide this.
Can I drive?
You will be advised not to drive while you are in the walker boot as it is not safe and you will not be covered by your insurance.
What can I expect?
You are likely to commence functional activity including driving at about 12 weeks following the injury. You will experience calf muscle wastage and sometimes localised swelling. However, this can improve to near normal with time. There may also be some discomfort and tendon stiffness. Occasionally, following conservative management the tendon heals in a slightly lengthened position which can lead to reduced push off strength when walking quickly or running.
There is a small risk of re-rupture of the Achilles tendon, and it can take 12 to 18 months to regain normal function.
If you have any concerns or questions, please contact the Physiotherapy department on 01482 608939.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

