- Reference Number: HEY005/2022
- Departments: Orthopaedics, Physiotherapy
- Last Updated: 31 May 2022
Introduction
This leaflet has been produced to give you general information about your injury. We understand you may not have seen a clinician face to face in fracture clinic however, most of your questions should be answered by this leaflet. If after reading it, you have any concerns or require further explanation, please do not hesitate to contact the fracture clinic team. Contact details are available at the end of this leaflet.
What is an ankle sprain?
An ankle sprain occurs when a ligament is forced into an abnormal position, causing it to overstretch. Ligaments are strong bands of tissue that connect one bone to another and help hold joints together.
In some cases, a small piece of this bone is pulled away with the ligament. This is called an avulsion. It is common for avulsion injuries to be treated in the same way as you would an ankle sprain.
The most common type of ankle sprain is when the sole of your foot turns inwards, overstretching the ligaments on the outside of your ankle and squeezing those on the inside.
What are the symptoms?
- Mild ache or a sudden pain
- Swelling and bruising
- Inability to move the ankle normally
- Difficulty putting weight on to the foot
How should an ankle sprain be treated?
In many cases, ankle sprains can be managed simply in a tubigrip bandage. However if you have significant pain or are struggling to weight bear you may be offered an ankle stirrup. This will provide some support and stability. You should wear whilst mobilising for up to 4 weeks. Whilst at rest, exercising the ankle or for hygiene purposes it can be removed.
What if I need pain relief?
To manage your pain, we advise that you regularly take simple pain relief, which can be bought over the counter. If you have allergies or conditions, which prevent the use of pain-relieving or anti-inflammatory medication, please seek advice from your doctor or a pharmacist.
What should I do in the first few days after the injury?
The most important initial treatment is aimed at controlling the pain and swelling by following the principles of RICE:
R REST
Complete rest is not advisable but it is important that you prevent putting the ankle under strain in the early stages of healing. If necessary, you will be given crutches to help you take some weight off the injured ankle.
The movements below should be practiced 10 times, three to four times every day. You may find initially you cannot move your ankle far but this will improve as the injury starts to heal:
To assist this movement, place a scarf or towel around your foot and gently pull your foot up, by pulling the scarf with your hands. Hold this position for five seconds. |
 |
| Now point your toes away from you and hold for five seconds. |  |
|
 |
I ICE
Ice will help reduce the pain in your ankle and so should be applied for 10 to 15 minutes before performing the exercises above. This will help to reduce the swelling.
There are many different ways in which ice can be applied however crushed ice, in the form of frozen peas for example, is the most effective. Whichever method you choose it is important that you wrap the ice in a damp towel, in order to prevent it from ‘burning’ the skin.
Please Note:
- Only use an ice pack on areas that have normal skin sensation i.e. where you can feel hot and cold
- Do not apply ice to an open wound
- Do not apply an ice pack to an area that has poor circulation
- When you apply ice to your skin, check the skin every five minutes and stop using it if:
- the area becomes white, blue or blotchy
- the area becomes excessively painful, numb or tingles
C COMPRESSION
You may have been given a tubigrip to wear to help control your swelling. It is important this is removed if you develop any signs of poor circulation such as tingling, numbness, blueness of the skin of the foot and increasing pain. The tubigrip should be removed when you go to bed at night as when you are asleep you cannot monitor these symptoms.
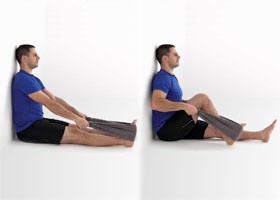
E ELEVATION
The ankle should be elevated above the level of the heart as much as possible, as this will reduce and prevent swelling.
 |
Carrying out the movements of the ankle described above, while the leg is elevated, may help to reduce any swelling further. |
What not to do
Consuming alcohol, massaging the injured area and applying heat can all be detrimental in the early stages of healing and therefore should be avoided. It is important to note that smoking may also delay the healing process.
Walking and exercise
It has been shown that your ligaments will heal quicker if you walk normally on the ankle as soon as possible after the injury.
 |
Normal walking means; that you strike your heel to the floor first, then rock forward onto your foot and lastly push off from your toes. |
Some patients will require crutches to achieve this normal walking pattern, but this will be assessed on an individual basis.
If you follow the basic advice, healing of the ligament normally takes around six weeks. However, everyone recovers from injuries at different rates and it is dependent on the severity of the injury and the presence of any other medical problems.
Once your pain begins to settle it is important to add into your regime the following exercises. These exercises will help you to regain full function, flexibility and strength. These will also reduce the risk of the injury reoccurring.
1. Stand facing a chair and step backwards with your injured leg.
 |
Keep this leg straight with your toes pointing forward and the heel on the floor.
Now bend your other knee until you feel a stretch in the calf of your injured leg. Hold this for 30 seconds and repeat three times per day |
2. From the position in exercise one move your injured leg forward but keep it slightly behind your other leg.
 |
Ensure that your toes point forward and bend both knees, keeping the heel of your injured leg on the floor.
You should feel a stretch in the calf of your injured leg. Hold for 30 seconds and repeat three times per day. |
3. Stand holding on to a chair, spread your weight equally over both feet and push up onto your toes as high as possible.
 |
Hold for five seconds and slowly lower. Repeat 10 times, twice per day.
Once this becomes easier you can increase the number of repetitions or progress to repeating this stood on the injured leg on its own. |
4. Stand on your injured leg and balance for as long as possible. To begin with, you may need to hold on to something solid to prevent you falling over.
 |
As you improve try doing functional activities such as washing the dishes or cleaning your teeth while you are standing on the one leg.
Try to hold your balance for up to 30 seconds. |
All photos with kind permission of ©Physiotec™
When can I return to normal activities?
When can I start driving again?
It is always good to check with your insurance company however we advise it should be safe to return to driving when:
- You are no longer using ankle stirrup
- You can walk comfortably
- You can perform an emergency stop
What about hobbies/sport?
If you participate in an active hobby then it is advisable that you do not return to this until you have full strength, full range of movement and you can walk briskly without experiencing pain and swelling.
If you play a sport you can practice sports specific activities; like dribbling or jumping. Build up these exercises gradually, in order to help regain strength and flexibility, before returning to full training sessions and competition.
Do I require a follow up?
Do I need to be referred to Physiotherapy?
If the fracture clinic team feel you need to be seen by the Physiotherapy team, you will be directly referred to physiotherapy from fracture clinic and if this is the case, you will have been informed of this in your telephone call following your Virtual Fracture Clinic appointment. You will receive a letter or phone call to book this appointment within 2 weeks of the referral being made.
If you have not received one within this time, please contact the physiotherapy department on tel: 01482 674880 between the hours 8.00am to 4.00pm, Monday to Friday. If there is no answer please leave a message and your call will be returned with the same working day.
Most of the time however, a referral to Physiotherapy is not needed, but if you have any concerns, are unable to follow the advice in this leaflet, or if you still have reduced movement, strength or function, East Riding GP patients can contact the East Riding MSK Physiotherapy service on tel: 01377 208300. Alternatively you can complete a self referral form on https://www.chcpmsk.org.uk/self-referral-form-introduction
Hull GP patients should call the fracture clinic number in the information below.
Do I need a Fracture Clinic follow up appointment?
A follow up appointment for fracture clinic is not required and you have been placed on a Patient Initiated Follow Up (PIFU) pathway. This means you will not have another appointment to be seen in fracture clinic.
If, however you have any problems or further queries relating to this injury within the next six weeks, you can contact us on tel: 01482 674378 during clinic hours 9.00am to 4.30pm Monday to Friday. Please do not choose an option and when prompted leave a message if there is no answer and we will aim to get back to you within the same working day. If you have not needed to contact us in the six weeks after your injury, you will be discharged and should seek advice from your GP.
This leaflet was produced by the Orthopaedic Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in May 2025.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

