- Reference Number: HEY295/2019
- Departments: Metabolic Bone Disease
- Last Updated: 31 March 2019
Introduction
This leaflet has been produced to give you general information about bone densitometry scans. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a bone densitometry scan?
A bone densitometry scan is a simple procedure that measures the amount of bone mineral in your bones. Measurements may be taken over your lower spine, hip, heel, forearm, hand or whole body depending on what your doctor requires. The scan is painless and does not usually need you to get undressed. The whole procedure normally takes less than 30 minutes.
Why do I need a bone densitometry scan?
A bone densitometry scan gives an indication of the strength of your bones and whether you have osteoporosis (brittle bone disease). You will also be asked to complete an osteoporosis risk questionnaire which will be used with your scan results. This is the best way of determining your future risk of fragility fracture. A fragility fracture is a particular type of break in a bone, caused by the bone being weak or fragile (brittle).
Can there be any complications or risks?
DEXA exposures
Your doctor needs to take an X-ray to help with your care. There are many benefits associated with the use of X-rays, such as your doctor being able to see what their eyes cannot (such as the density of your bones). This is much safer than using invasive techniques such as surgery.
X-rays are exceedingly safe but there is a small risk involved. You will receive a negligible dose of radiation which carries a tiny (less than one in a million) chance of side effects. Your doctor will never take an x-ray unless the benefit to you exceeds the minimal risk. This dose of radiation is so small that it will be equivalent to what you receive in a few days from natural background radiation that is present in the surrounding environment.
You should contact the Centre before your scan appointment if there is a chance you may be pregnant.
How do I prepare for the scan?
- Please wear clothing that has no metal parts between the chest and knees and is not bulky around the waist or hips. If possible do not wear jeans, an underwire bra or a long-line bra.
- Please bring the completed osteoporosis risk questionnaire with you as this will speed up your visit.
- Please contact the Centre if you have an appointment for a nuclear medicine scan, barium X-ray or other X-ray procedure involving an injection of dye in the two weeks before your bone density appointment, as these tests may interfere with your bone density scan.
What will happen?
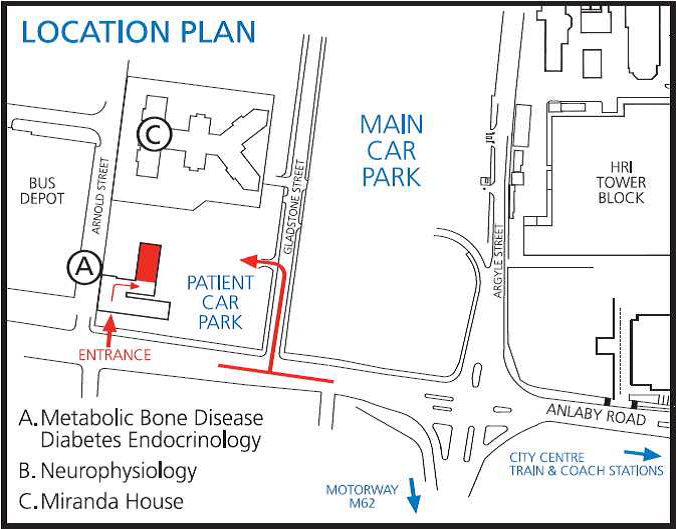
You should attend the Centre for Metabolic Bone Disease on the Hull Royal Infirmary site (map enclosed). You will be greeted by one of the receptionists and a medical technician will perform the scan.
The scan generally involves you lying on your back for a short time whilst the scanner moves above your abdomen and hips. During the scan of your spine, your legs will be raised onto a foam block to ensure that your spine is flat on the bed.

The scanner will not touch you and you will not feel anything. You will not go into a tunnel. Your visit for the scan will take about 30 minutes. You will not usually need to lay flat for more than 10 minutes. The technician performing the scan will be present while you are being scanned.
What happens afterwards?
- The results will be sent to your doctor or Consultant.
- Treatment advice and monitoring will be suggested where applicable
- Some results may take slightly longer if they require a clinical comment
Directions to the Centre for Metabolic Bone Disease
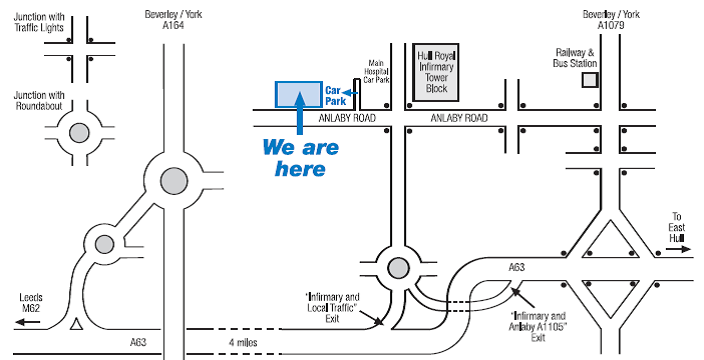
West – follow the A63 east to Hull, going under the Humber Bridge and on past St. Andrew’s Quay. Come off the A63 at sign Infirmary/Local Traffic. At the bottom of the slip road take the second exit off the roundabout onto Rawlings Way and follow road to next junction. Turn left at this junction onto Anlaby Road and take the first right into Gladstone Street. Turn left into the H S Brocklehurst Building Car Park. Note, do not follow the signs for the main hospital car park. The entrance to the building is on Anlaby Road.
North – take the A164 from Beverley. Continue following the signs for the Humber Bridge until reaching the Humber Bridge Roundabout. Do not cross the bridge. Instead, take the third exit off the roundabout, sign posted Hull (A63). Go straight across the next roundabout keeping in the left hand lane and follow signs for Hull (A63)/Bridlington (A165). Now follow directions as from West (as above).
South – follow the A15 over the Humber Bridge. At the first roundabout after the bridge turn left, and follow the road to the next roundabout. Keeping in the left hand lane go straight across the roundabout and follow signs for Hull (A63). This slip road will take you onto the A63. Now follow directions as from West (as above).
East – follow the A1033 (Hedon Road). Go over the Myton Bridge and straight ahead at the traffic lights, passing Hull Marina on the left. Carry straight on at the next two sets of traffic lights. Take the next slip road on your left signed,” Infirmary/Anlaby (A1105)”, the Smith and Nephew factory and offices are to your left. Take the third exit off the roundabout onto Rawlings Way. Continue to the next junction and turn first left onto Anlaby Road. Take the first right into Gladstone Street and left into the H S Brocklehurst Building Car Park. Note, do not follow the signs for the main hospital car park. The entrance to the building is on Anlaby Road.
For information on bus routes call: tel: 01482 222222
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact: Centre for Metabolic Bone Disease on tel: 01482 675340
PLEASE BE AWARE THAT IF YOU ARE MORE THAN 15 MINS LATE THE TECHNICIAN WILL HAVE ANOTHER PATIENT WAITING AND THERE IS A CHANCE WE MAY HAVE TO RE-BOOK YOUR APPOINTMENT.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.