- Reference Number: HEY1145/2023
- Departments: Ophthalmology Department, Orthoptic
- Last Updated: 31 December 2023
Introduction
This leaflet has been produced to give you general information. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is Brown’s Syndrome?
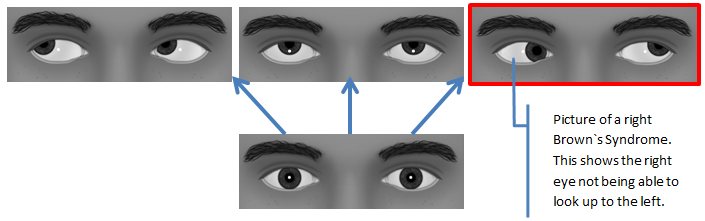
There are six muscles around each eye which allow the eyes to move in different directions. Brown’s Syndrome is a condition where one of the muscles that lifts the eye upwards (superior oblique muscle) does not work as it should.
The superior oblique passes through a ring of cartilage called the Trochlea. This acts as a natural “pulley” system to help the eye to move. In Brown’s Syndrome, there is a defect at the site of the pulley-trochlea complex which does not allow the muscle to pass through freely. This results in an inability to look upwards and inwards as shown in the picture below. This can give the impression of a squint when looking up and into the corner. It usually only affects one eye, but can occur in both eyes. Some patients notice a “click” or “clicking” sensation when they try to look upwards and inwards.
What is the cause of Brown’s Syndrome?
Brown’s Syndrome is usually present from birth. It may be caused by the muscle being too short, inelastic, thick, a swelling on the muscle tendon, or a ‘miss-wiring’ of the muscle fibres themselves. Most cases occur without any family history.
It is possible for Brown`s Syndrome to be acquired in later life, however this is usually as a result of surgery, injury, or inflammation in the area between the eye and the nose.
Can this impact vision and why do I need to attend appointments?
Brown’s Syndrome does not affect the vision directly, and in most cases individuals will use both eyes together normally. Individuals with the condition may find it uncomfortable to look up into the area which is affected. In some cases an individual with Brown’s Syndrome may adopt a very subtle head posture to make it more comfortable. Any head posture should not be discouraged. In some cases there may be an associated squint or need for glasses.
In children it is advisable to attend orthoptic appointments so that your Orthoptist can ensure that the vision is continuing to develop normally. Your Orthoptist may also be able to suggest any adjustments that may make some things easier for you/your child.
Can there be any complications or risks?
Brown’s Syndrome tends to improve over time therefore children who are born with the condition do not require treatment unless there is an associated squint or a need to wear glasses. Surgery may be considered if the squint is large and/or the head posture used to compensate is large and/or uncomfortable. This would only be in marked cases and would need to be discussed with your Paediatric Ophthalmologist (children’s eye doctor).
In adults who develop Brown’s Syndrome with symptoms of double vision (diplopia), a plastic prism may help relieve symptoms by joining the two images together. A temporary prism may be fitted onto your glasses initially but can later be incorporated into them if required. In some rare cases surgery may be considered, again this would need to be discussed with your Ophthalmologist.
How can I help if my child has Brown’s Syndrome?
Looking up can be difficult for those with Brown’s Syndrome. This can be particularly difficult for children as the world is set up for adult height. As children grow taller this naturally becomes less of a problem.
In a classroom setting, sitting on the floor for story time or to look at the whiteboard can force the child to look up. This may cause discomfort and make it difficult for them to pay attention. Your child will be more comfortable when sitting at eye level with the teacher.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Orthoptic Department on tel: 01482 816605