- Reference Number: HEY1491/2024
- Departments: Trustwide - Adult
- Last Updated: 31 August 2024
Introduction
This leaflet contains information about hepatitis B. It explains how you may have been infected and the symptoms, diagnosis, and management options. It has been developed by the hepatitis team, which includes doctors, nurses and pharmacists.
If you have any questions, please do not hesitate to contact us for further advice or resources. Contact details are at the end of the leaflet.
What is Hepatitis B?
Hepatitis B infection is caused by the hepatitis B virus (HBV), which can infect your liver. It spreads through blood and other body fluids. It can damage the liver, and if it’s not treated it can lead to serious problems like liver cirrhosis or cancer.
Some people get rid of the virus on their own, but if it stays in your body for more than six months, it is called chronic hepatitis B. This can last for many years without causing any symptoms.
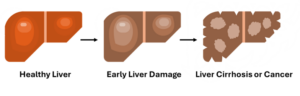
Around one in three people with hepatitis B will develop liver cirrhosis or cancer without treatment. Hepatitis B treatment can stop new liver damage and allow the liver to slowly recover.
Around 240 million people worldwide have chronic hepatitis B. It is more common in Africa, Asia and Eastern Europe than in Western Europe, North America or Australia. Hepatitis B is one of the main causes of liver cancer across the world.
How did I get Hepatitis B?
Most adults with chronic hepatitis B were first infected as babies or young children, but some people catch it as adults. It spreads in different ways, such as:
- From a mother to her baby at birth
- Living with someone who has hepatitis B infection
- Growing up or living in parts of the world where hepatitis B is common
- From infected blood or blood products, or through healthcare if items were not properly sterilised
- Sharing toothbrushes, razors or needles for drugs, tattoos or piercings.
- Unprotected sex (sex without a condom) with an infected person
How can I avoid giving Hepatitis B to others?
The virus can spread through blood and body fluids. The amount of virus can vary between people and change over time. The best thing to do is to see a hepatitis specialist who will measure how much virus is in your blood and discuss any risks.
Here are some ways you can protect others:
- Make sure your family, close contacts and any regular sexual partners have been vaccinated against hepatitis B if they are not already immune. This needs to be arranged through their GP.
- Don’t share items like needles, razors, or toothbrushes or expose other people to your blood.
- Use condoms until your partner is tested and vaccinated. However, kissing and breast feeding do not transmit hepatitis B.
- Pregnant women can give hepatitis B infection to their children during the birth, but this can be prevented through vaccination and medication. If you are pregnant, please ensure you attend your maternity and hepatitis clinic appointments.
- Skin-to-skin touch does not transmit hepatitis B unless the skin is broken. Cover any cuts and clean up blood spills yourself with bleach.
- If you work in healthcare, you should inform your occupational health department, but most healthcare workers can continue their work without any changes to their duties.
What symptoms might I have?
Most people with hepatitis B feel fine and don’t have any symptoms. If you do have symptoms, they might include:
- Tiredness, fever, general aches and pains
- Loss of appetite
- Feeling or being sick
- Tummy or abdominal pain or swelling
- Dark urine
- Light brown to light grey bowel movements
- Yellowing of the skin or eyes, called jaundice
- Hepatitis B virus can damage the liver without making people feel unwell in any way. You should always talk to a health professional if you have any new symptoms, you are worried about.
How is Hepatitis B diagnosed?
We test for a protein in your blood made by hepatitis B virus, called hepatitis B surface antigen (HBsAg). If this test is positive, it means you have hepatitis B, and you will be referred to the hepatitis team.
To understand the stage of your Hepatitis B and your liver health, you will likely undergo the following:
- Fibroscan, to check for early liver damage
- Ultrasound scan to look at the shape of your liver
- More blood tests to understand how much virus is in the blood and whether treatment is recommended.
How is Hepatitis B treated?
There is no cure for hepatitis B yet. Sometimes the body can control and clear hepatitis B by itself, but this is unusual. About 1 in 100 patients clear hepatitis B by themselves every year, and we can’t tell who these people will be. Medication can control the virus and stop more liver damage. Not everyone needs medication, it depends on your test results.
If treatment is recommended, we will discuss the best options with you.
The main medications are called tenofovir and entecavir. These drugs stop the virus multiplying in your body.
How is the medication supplied?
You can only get hepatitis B medication from your hospital specialist team, not from your regular doctor (GP). You will also need regular blood tests every six months. Please keep your appointments.
If you cannot keep your appointment or if you are running out of medication please call the hepatitis secretaries. Contact details are at the end of the leaflet.
How can I keep my liver healthy?
You can keep your liver healthy by:
- Eating a healthy, balanced diet and staying at a healthy weight
- Not drinking alcohol
- Not smoking
- Exercising regularly
- Drinking coffee, which may reduce the risk of liver disease and liver cancer
- Attending your clinic and scan appointments.
- Taking any medication prescribed for hepatitis B regularly and as recommended.
What if I’m pregnant, or want to have a baby?
People with hepatitis B can have a healthy pregnancy and breastfeed. You will need to come to hepatitis clinic during the pregnancy. If you are taking hepatitis B medication please keep taking it, do not stop without talking to your hepatitis team as this can be dangerous.
Babies born to mothers with hepatitis B need to be vaccinated on the day they are born. They need a second dose at one month old, given by the health visitor or GP. Hepatitis B vaccine is also given as part of the routine childhood immunisations at 2, 3 and 4 months old. The baby should be tested for hepatitis B and given a final dose of hepatitis B vaccine at 12 months old.
Frequently asked questions:
Why should I go to my appointments?
Whether you are on treatment for hepatitis B or not, it is important to keep all your appointments so the medical team can check your liver health and adjust your treatment if needed.
If you are on treatment then more medication can be given, your GP is not able to prescribe these specialist medications.
Who is included in the specialist healthcare team?
- Consultant (specialising in Hepatitis B) and resident doctors
- Specialist Nurses
- Pharmacists
- Virologist
The team works together to make sure you have the best monitoring and management of your hepatitis B. The doctor or nurse who sees you will write to your GP about your treatment plan. We usually send you a copy of the clinic letter, if you do not want to be sent a copy please tell the doctor or nurse who sees you in clinic.
Where do I get my medications from?
Hepatitis B medication is prescribed in the hospital and only supplied by the hospital pharmacy, it is NOT supplied by your GP or community pharmacy. Please contact the hepatitis secretaries if you are due to run out in 2 weeks and do not have an appointment.
What monitoring is needed?
Blood tests are done at least every 12 months, more often for people taking hepatitis B medication or having close monitoring. You may also need regular scans to check your liver health. Your hepatitis team will develop a personalised care plan for you and let you know the monitoring required.
What if I plan on moving home?
Within Hull/East Riding – please let the clinic reception or hepatitis secretaries know the new address so we can send medication and letters to the correct address.
Different part of the UK – please let us know as soon as possible as we will need to transfer your care to the local service for your new address.
Different part of the world – please let us know before you leave so we can provide information and enough medication to allow time for you to find a new hepatitis team.
What if I plan on leaving the UK for more than a few months?
Please discuss this with your specialist team or the hepatitis secretaries so we can arrange appointments and medication if needed.
Is there any research looking at a cure for HBV?
There are studies trying to find a cure for hepatitis B, but it will probably be many years before one is available. Please let your hepatitis team know if you might be interested in taking part in hepatitis B research in future.
Further information and support
For more information you can:
Call the Hepatitis secretaries on tel: 01482 622267
or
Visit the British Liver Trust website at www.britishlivertrust.org.uk
Keep all medicines out of the reach of children.
Never share your medication with others, it may harm them even if their symptoms are the same as yours.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Department of Infection.

