- Reference Number: HEY617/2024
- Departments: Endoscopy
- Last Updated: 30 April 2024
Introduction
This leaflet has been produced to give you general information about your procedures. Most of your questions should have been answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
Why have these procedures been arranged for you?
You will have seen your doctor about some symptoms that have been troubling you. Your doctor has arranged for you to be seen by a specialist (or representative) in a clinic.
Your doctor or your specialist feel that these examinations are the best way to investigate your symptoms. In this way the whole of the lining of your gullet (oesophagus), stomach, the first part of your small intestine and the large bowel is seen at one visit.
The benefits of these examinations include the ability to take biopsies to analyse small parts of tissue which may be abnormal. The tissue is removed painlessly with a tiny pair of forceps and taken for analysis in the laboratory. A colonoscopy also enables the removal of polyps without the need (in the vast majority of cases) for an operation. This can usually be done at only one visit.
What is a combined Upper GI endoscopy and colonoscopy?
These combined procedures may help to find the cause of your symptoms. An upper GI Endoscopy is a test that allows the endoscopist to look directly at the lining of the gullet (oesophagus), stomach, and first part of the small intestine (duodenum). Other names used for an upper GI endoscopy you may hear are OGD and Gastroscopy. The colonoscopy is an examination of the large bowel (colon). The upper GI Endoscopy will commonly be the first procedure undertaken but there is no set rule and the order may depend on the order the endoscopist considers is best for you.
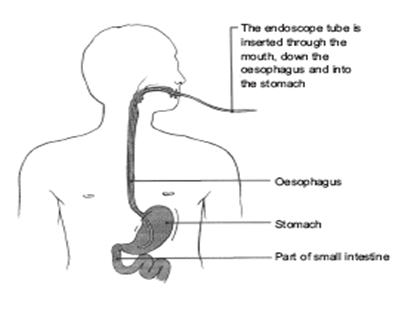
Upper GI Endoscopy
A slim flexible tube with a light on the end is gently passed from your mouth into your stomach. Pictures from the tube are shown on a television monitor and a clear view of your gullet, stomach and duodenum can be seen.
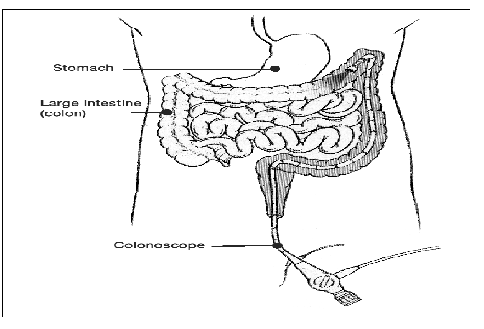
Colonoscopy
This is an examination of the large bowel using a long, flexible tube called a Colonoscope. The tube allows the colon to be viewed directly and for pictures of the lining and samples of the tissues to be taken.
The patient pictures are reproduced with the permission of Health Press Limited from Neild P, Gazzard B. Patient Pictures – Gastroenterology, Oxford Health Press, 1997.
What if I refuse to have the gastroscopy or colonoscopy?
This is your choice and there might be alternative examinations we can use instead. This will not alter the manner in which we treat you and your standard of care will not change. However, your plan of care and treatment may change, as it is possible that some important information will be unavailable. Please discuss this with your consultant or endoscopist.
What are the alternatives to these procedures?
X-ray examinations are available as alternative examinations but sampling of biopsies and the treatment of polyps is not possible. X-rays can often tell us if an area looks abnormal but they cannot always tell us what the problem is.
Does Upper GI endoscopy have any risks?
All endoscopies carry a very small risk of haemorrhage (bleeding) or perforation (making a hole) of the bowel, stomach or gut. If this occurs, you will need to be admitted to hospital as sometimes an operation is needed.
If you have sedation other rare complications include a reaction to the sedation drugs. Some people, for reasons we still do not fully understand, are particularly sensitive to this drug. The breathing can be too shallow and too slow. In these cases we stop the examination, give more oxygen and if required we can give an antidote, which reverses the effect of the sedation. This is usually all that is needed and the person recovers with no ill or lasting effects.
In some cases, when people have another serious illness e.g., heart disease, stroke, unstable angina, severe asthma or chronic bronchitis, the sedation drug can cause difficulty in breathing. Severe reactions are rare however a drop in oxygen levels occurs in 70 patients out of 100 and is why we monitor breathing and heartbeat throughout; and why we give oxygen by nasal tubes.
If you have a known allergy or reaction to sedatives and anaesthetics, please let the endoscopist or your nurse know.
In addition there is a possibility of developing aspiration pneumonia (fluid in the lungs). There is also a slight risk of damage to crowned teeth or dental bridgework. Common problems, which are not serious, include bruising from the sedation needle, a sore throat and bloating. If you would like to know more, please ask your nurse or endoscopist about the hospital’s complication rate.
Does colonoscopy have any risks I should know about?
Yes, risk means complications may occur. It is important to note that serious complications during colonoscopy are rare. Complication rates, that is, how often complications occur, vary across the United Kingdom. If you would like to know our rates for serious complications this can be discussed with you during your consultation. Complications can be described as minor (mild) or major (serious):
Minor complications:
These complications are common and expected but do not last for long and do not cause serious harm.
They include feeling bloated after the examination with trapped wind, feeling faint and dizzy, cold sweats and occasionally feeling sick.
We do keep a close eye on you in recovery and in the majority of patients these subside either very quickly (15 to 20 minutes) or over a couple of days. Over this time bloatedness is common and comes and goes. As long as you are passing wind and going to toilet, this will settle down.
There is a small risk of bleeding from the bottom after colonoscopy. The entrance to your bottom, the anus, does have a very good blood supply and this is where piles are often found. The insertion of the camera can cause a little bleeding. This should only be ‘spotting’ on the toilet paper or drops in the toilet bowl. It may take some days for this to subside.
Major complications:
These are complications, which can be serious, may lead to admission to hospital and sometimes an operation. On rare occasions these can be life threatening, especially in people with serious unstable cardiovascular or lung problems.
It is important to be aware that major and serious complications are rare.
Complications, which can become serious and life threatening include:
Perforation of the bowel
A small tear may occur through the bowel wall. This can especially occur in thin, diseased bowel or when polyps are been removed. If it occurs you may begin to feel unwell, feel nauseous or vomit, your tummy may become hard, swollen and painful. You may feel hot and shivery. These symptoms can occur within minutes of the perforation or may slowly develop over days.
If you have any of these symptoms YOU MUST CONTACT your doctor or the hospital Endoscopy Department, or Ward 100 HRI (out of hours) as soon as possible.
Bleeding
This can occur especially after the removal of polyps. Although great care is taken to ensure there is no sign of bleeding after a polyp is removed, the contraction of the bowel after colonoscopy when getting rid of wind or when the bowels are next opened can cause the area where the polyp was to bleed.
You should expect a little bleeding, such as ‘spotting’ on the toilet paper or small drops in the toilet bowl. This usually subsides quickly. If bleeding begins to increase and large clots of blood are seen or you begin to feel unwell or faint, please contact your doctor immediately for advice and help.
Recent evidence puts the risk of perforation, sometimes accompanied by bleeding at 1 in 1000. This can be higher with the removal of large, difficult polyps, especially in the caecum. This is usually the thinnest part of the large bowel.
In some cases, when people have another serious illness e.g., heart disease, stroke, unstable angina, severe asthma or chronic bronchitis, the sedation drug can cause difficulty in breathing. This is rare and is why we monitor breathing and heartbeat throughout; and why we give oxygen by nasal tubes.
Entonox
You may decide that sedation is not for you or in some cases sedation may not be appropriate e.g. if you have a serious underlying condition that makes sedation unsafe or you have no-one to look after you after your procedure. There is an alternative to sedation.
For the upper GI Endoscopy you can have your throat numbed with a local anaesthetic. The advantages are:
- It is the safest way to have the procedure
- No long lasting drowsy effects for the day.
- You do not need someone to take you home or stay with you
- You will be able to understand any advice, instructions and results.
For the colonoscopy Entonox can be used and is also known as ‘gas and air’. Entonox is a gas that can help relieve pain. It is used by inhaling the gas through a mouthpiece. It means that you have control over how much or how little you take. One of the advantages of Entonox is that it is quickly expelled from the body. This means that you will be able to drive 30 minutes after the procedure and will not need someone to collect you or stay with you overnight. There are some rare cases in which Entonox would not be safe to use. If you wish to have Entonox during your procedure please inform the nurse during your assessment. You will be asked a series of questions by the nurse to make sure you are suitable for Entonox. It is not suitable for patients taking the drug Methotrexate.
Preparing for both Upper GI endoscopy and colonoscopy
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination. Complete the health questionnaire sent/given to you as fully as possible.
The preparation for your procedures will start the day before your appointment
To allow for a clear view of your stomach and first part of the intestine, it needs to be empty and free of food. To be able to see the lining of the large bowel it will need to be empty and free of faeces (stool). To do this you will be asked to stop eating prior to your procedure, the time at which you stop eating will depend on your appointment time. To ensure that your large bowel is empty we will send you sachets of a special powder (bowel preparation) to mix with water and drink. Instructions for how and when to take these sachets, what to eat and when to stop eating should have come with your appointment time. If not, contact the Endoscopy Department.
This ‘bowel preparation’ will cause you to have diarrhoea. Sometimes it works within 1 to 2 hours but both sachets need to be taken to be effective. You must drink plenty of fluid during this time. Avoid ‘fizzy’ drinks. You can lose a lot of fluid and you can easily become dehydrated making you feel unwell.
When you have finished drinking the second sachet mix you may continue drinking clear fluids (see instructions sent with the sachets) up until four hours before your procedure time.
You must ensure that you have nothing to eat or drink for four hours prior to your appointment time. Sometimes people feel sick and even vomit during this test. By keeping your stomach empty there is less likely of any fluid entering your lungs should you vomit.
If you have diabetes (especially taking insulin) or you have serious heart, lung or kidney problems, or concerned that a health problem you have may be affected, then contact the Endoscopy Department at the hospital where you are having your examination.
- Latex – Please inform the department if you have a confirmed latex allergy as this will affect your appointment time.
- Creutzfeldt-Jakob disease/variant Creutzfeldt-Jakob disease (CJD) – Please inform the department if you have been notified that you are at risk of CJD/vCJD for public health reasons.
- Pregnancy – It is important that you inform us if there is a possibility that you may be pregnant. Any information you share with us will be kept strictly confidential.
- Medical devices – If you have a pacemaker or implantable cardioverter defibrillator (ICD) that has not been checked within the last six months please telephone the department as soon as possible. If the device has been checked in the last six months then all you need to do is inform the nurse on admission of the device and date last checked. Please contact the department if you have a pacemaker.
Due to the above or other individual reasons, we do admit some people to hospital for preparation and colonoscopy.
Due to the nature of the examination we ask you to undress. A private changing area is provided. Although a gown and privacy shorts are provided, you may also wish to bring a dressing gown with you.
With your appointment letter, a health questionnaire will be sent. Please complete this to the best of your ability. This forms an important part of assessing your ‘fitness’ for the procedures and the potential for complications to occur, so that action can be taken to eliminate or reduce these risks.
If your health has deteriorated whilst waiting for this examination, please inform your Endoscopy Department.
Your co-operation with the above is extremely important, without this your procedures could be delayed.
Where will I have my procedures?
The procedures will be performed in the Endoscopy Department. It will be done at Hull Royal Infirmary or Castle Hill Hospital depending on where your consultant is based. Please make sure you go to the correct Endoscopy Department. Directions will be given with your appointment letter.
All the staff will endeavour to make your stay as easy and dignified as possible. Please do not be afraid or embarrassed to ask questions.
Who will perform my procedures?
It may be your consultant or another experienced gastroenterologist who is experienced in performing these examinations. In these cases, your consultant will be sent a copy of the result. Trained and experienced nurse specialists (nurse endoscopists) also perform these tests. Their training has been through a specialist course.
This Trust is a teaching hospital and has commitments to train both doctors and nurses in all aspects of endoscopy and care. Occasionally doctors or nurses who are undertaking endoscopy training may perform your procedure. An experienced endoscopist will supervise them. Your permission will be requested in advance for this. You may decline and the supervising endoscopist will perform the endoscopy.
Should I take my tablets whilst I am preparing for the procedures?
If you are taking tablets prescribed by your doctor or other specialist, you should continue to take these as normal. There are some medications that may need to be stopped or reduced for a period of time before your procedures. You will be told if this applies to you.
If you are taking any of the following medications, please contact your Endoscopy Department for further advice and instructions.
- CLOPIDOGREL (PLAVIX) – Please inform the department if you are taking these tablets as these may need to be stopped prior to your procedures.
- WARFARIN – These are blood-thinning tablets and may have to be stopped for a period of time before the day of your procedures due to the risk of bleeding.
- INSULIN – For some people with diabetes, we may need to admit them to hospital for the day and night before the test. There is a risk that the bowel preparation for the examination and restricted diet could make the control of your blood sugar difficult and make your diabetes unstable.
- IRON – If you take iron tablets then these are usually stopped for one week before the colonoscopy. Iron coats the inside of your large bowel making it very dark and difficult for the endoscopist to see anything. It is important to stop iron otherwise your colonoscopy will be cancelled and another appointment made.
If you take any of the following blood thinning tablets please contact the Endoscopy Department before your appointment for further advice: APIXABAN, RIVAROXABAN, DABIGATRAN, ARGATROBAN, OR EDOXABAN
If you have any concerns about whether to take your medications before your colonoscopy, contact your Endoscopy Department.
What happens to me in the Endoscopy Unit?
Our friendly staff will greet you on arrival. They will let your nurse know you have arrived. Occasionally there may be a delay in your appointment time, due to an emergency taking place. If there are any delays you will be notified as soon as possible and be kept informed.
We will explain what to expect. You will need to remove your lower clothing and will be given a gown and privacy shorts to change into. A place to do this will be provided, ensuring your privacy. If you have a dressing gown please bring this with you.
We will ask questions about your general health and work through the health questionnaire that you kindly completed for us. Please feel free to ask questions.
We will check your blood pressure, pulse, oxygen levels and weight, before your procedures.
These procedures commonly involve the giving of intravenous sedation – a combination of drugs, which makes you relaxed and provides pain-relief. To be able to do this a needle is inserted in a vein in your hand or arm. This is removed once the examination is finished and you have recovered from the sedation.
If you have opted for Entonox the nurse will explain how to use it.
Your endoscopist and nurse will discuss the examination with you and will answer any questions you or a family member has. You will then be asked to read and sign the consent form. At any point during the procedure you can withdraw your consent and ask for the procedure to stop. If this happens the endoscopist will stop the test and take the scope out.
If you need glasses to read, please keep them with you at all times do not leave them with a relative or tucked away in a bag or pocket.
You are then taken through into the examination room. You will be asked to lie on your left side on the examination trolley. Your belongings will be put in a plastic bag and will be with you all the time. Any valuables should be left at home.
Once in position, your nurse will attach a finger probe, which monitors your oxygen levels and pulse throughout and after the examination.
If you are having the local anaesthetic spray to your throat, this will be administered first. The upper GI Endoscopy is most commonly performed first. When you are ready the nurse looking after you will gently place a plastic mouth guard into your mouth. This protects your mouth and teeth. You may feel the tube gently slide over your tongue and down your gullet. It will not hurt or interfere with your breathing but it can feel unusual and uncomfortable. If you get a lot of saliva your nurse will clear it with a slim suction tube. You may feel the tube move around in your stomach. Some air will be passed down the tube to inflate your stomach to allow for a clear view. The test normally takes five minutes or less.
When the Upper GI Endoscopy procedure is completed the nurse caring for you will re-position the trolley that you are on ready for the next procedure. All the equipment used for the first procedure will then be replaced for the second procedure. If you are having sedation, further sedation may be given at this time. If you are having Entonox you will be instructed on how to use it now.
The endoscopist will examine your bottom with a finger. This allows lubricating jelly to be applied and to examine the first few centimetres of the large bowel, which is sometimes not seen by the camera.
When the camera is inserted into your bottom, air is gently passed into the bowel.
This opens up the bowel so the endoscopist can see where they are going. At first you may feel that you want to go to the toilet. You may feel a little anxious and embarrassed that you will pass a motion.
DO NOT WORRY
The first part of the large bowel begins to stretch. This sends messages to your brain telling you to go to the toilet. It is the air that causes this feeling. You will not mess yourself. As the camera is gently inserted further into the large bowel, this feeling should ease, but may not totally go away.
The large bowel is not straight. It has twists and turns. Sometimes this makes it difficult to steer the camera around these bends. In these cases, more air is used and sometimes a bit more pressure to the end of the camera to help push and pull the camera around the bend.
This can cause discomfort and varies from person to person. It may be an ache and you may feel bloated, especially under the ribs. Instinct tells you to hold your breath until it passes. Try to relax and control your breathing, with good gentle, slow deep breaths. Your nurse looking after you will help.
Sometimes it can be quite painful. You must let your nurse and the endoscopist know. We can stop and remove some air. The colonoscopy takes about 20 to 30 minutes.
What happens when the procedures are finished?
You will be asked to stay on your side and as the trolley is moved into the recovery room. Here a nurse will continue to monitor your recovery this will involve checking your blood pressure, pulse and oxygen levels at regular intervals.
Gradually, as you recover, you will be advised to get rid of any ‘wind’ that may be trapped in your large bowel. We do appreciate that this can be embarrassing but it is important you do ‘let it go’.
You will eventually be able to sit up and you will be offered a drink. As you continue to recover you will be able to get dressed fully again and rest in a chair where you will be offered a drink and a biscuit.
Please take care. Initially you may feel dizzy and a little disorientated when getting off the examination trolley. As the effects of the throat spray wear off you may have a sore throat.
If you live alone or you do not have anyone who can be with you, please contact your Endoscopy Department so that other arrangements can be made.
Do I need someone with me after my procedures?
If you have sedation yes, this is very important. The sedation given can have effects, which last 24 hours after the colonoscopy. You can become forgetful and also sleepy again. Your test may be cancelled if you do not arrange to have someone to collect you and stay with you for the next 24 hours.
We strongly recommend that for the next 24 hours you:
- Do not drive
- Do not return to work or operate machinery
- Do not sign any important or legal documents
- Are not left alone, you may be at risk of injuring yourself
- Are not left alone to care for children
If you choose to have your procedure with Entonox and local anaesthetic throat spray you do not need someone to take you home.
If you have undergone a polypectomy, it is recommended that you avoid air travel, especially long haul flights, for a duration of two weeks following the procedure.
Will I be told what was found and what happens next before I leave the Endoscopy Unit?
Yes. Your nurse and the endoscopist will explain the results to you. If you have sedation you may forget what has been said. This is why it is important to have someone with you. The information will be written down and further supporting information in the form of leaflets will be given if required.
Will I ever need the procedures again?
This will depend on the reason for the procedures, what is found and whether it was possible to complete them. If polyps are found during colonoscopy, they are removed. Depending on the type and size of the polyp, the bowel may need to be checked at regular intervals to ensure the polyp has been completely removed and no new ones have grown.
For some, despite following instructions and taking the bowel preparation to empty the bowel, the view with the camera is poor. The endoscopist cannot be certain that the entire large bowel has been seen. In these circumstances, a repeat colonoscopy is needed and an alternative bowel preparation may be prescribed.
Occasionally, people’s bowels have very severe twists and turns and it becomes too difficult for the endoscopist to get the camera all the way round. Sometimes, despite pain relief medication, it is too painful for the patient and they ask the endoscopist to stop. In these cases a barium enema x-ray is needed to examine the rest of the large bowel.
If you do need a repeat upper GI endoscopy or colonoscopy, do not worry. It is not often because something serious has been found but usually for the reasons described above.
Further information
If you require further information about your test your doctor, consultant, and the Endoscopy Department is a valuable source of information. These are free of charge.
Further information about your rights with regards to consent can be found in the following documents:
- Department of Health (2001), Guide to Consent for Examination or Treatment
- Department of Health (2001), Consent – What you have a right to expect
- A Guide for Adults. (Available from the Endoscopy Department)
- A Guide for Relatives and Carers. (Available from the Endoscopy Department)
Visit the Department of Health’s website at: www.doh.gov.uk and, for consent: www.doh.gov.uk/consent
Useful contact numbers:
The Endoscopy Department, Castle Hill Hospital, tel: 01482 622069, Monday to Friday from 8.00am to 5.00pm
The Endoscopy Department, Hull Royal Infirmary, tel: 01482 674790, Monday to Friday from 8.00am to 5.00pm
Ward 100 Hull Royal Infirmary Out of hours, tel: 01482 674860
What do those words in the leaflet mean?
- Biopsy: A sample of tissue is taken for analysis.
- Caecum: The first part of the large bowel; this is joined to the small bowel.
- Consent: This is the agreement between you and the endoscopist. You are agreeing to have investigations or treatment and that you understand the purpose, benefits, alternatives and risks. You and the endoscopist during this process usually sign a consent form.
- Colonoscopy: The examination of the inside of the large bowel using a long, flexible camera.
- Duodenum: The part of the gut leading from the stomach.
- Endoscopy Department: The place where your procedure takes place.
- Endoscopist: This can either be your consultant, an experienced and trained doctor or an experienced and specially trained practitioner.
- Gastroscopy: Endoscopic inspection of the stomach (see endoscope).
- Oesophagus: The gullet. The pipe leading from the mouth to the stomach
- Perforation: A rare, but possible risk in which a hole or tear is made through the large bowel.
- Polyp: A common, benign (not cancer) growth arising from the lining of the large bowel. They take some years to develop. Some polyps, depending on their size and type, have the potential to turn cancerous.
- Polypectomy: The removal of a polyp usually performed at the same time as the colonoscopy.
This leaflet has been written with the help, support, advice and collaboration of:
- Consultants in the Academic Surgical Department and the Department of Colorectal Surgery
- Consultants of the Department of Gastroenterology
- Staff of the Endoscopy Departments at Castle Hill Hospital and Hull Royal Infirmary
The patients and carers who have shared their experiences of colonoscopy with me and helped in auditing the information produced for readability, understanding and user-friendliness.
You will be given an information checklist to complete and bring with you as outlined in the link below:
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

