- Reference Number: HEY-687/2023
- Departments: Ophthalmology Department
- Last Updated: 31 May 2023
Introduction
This leaflet has been produced to give you general information about the risks and benefits about corneal graft surgery. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is the cornea?
The cornea is the curved ‘window’ at the front of the eye, which must be clear to enable you to see. The cornea can become hazy due to disease or injury; this will mean that you can no longer see clearly through it. A corneal graft (transplant) operation may be performed to replace the diseased cornea.
What is a corneal graft operation?
There are several types of corneal graft (transplant) operations; your suitability for this operation will be discussed with you by your Consultant.
A corneal graft operation is a transplant operation that involves the removal of the full thickness of your central cornea (penetrating keratoplasty) and it is replaced with a cornea from a donor. This donor cornea is taken from the healthy eye of a person who has died (where permission has been given by the deceased prior to death, or more usually by the family).
In some cases a partial thickness corneal graft can be performed (deep anterior lamellar keratoplasty) where only the diseased layers of the cornea are removed and replaced with healthy new layers from a donor. There will be a few stitches in places to hold the graft in its place which will be removed in a few months after the operation; the timing of this is based on the healing process of your eye.
In approximately 10% of cases of patients having a lamellar keratoplasty the tissues tear and conversion to penetrating keratoplasty is required. Replacing deeper parts of the cornea is called an endothelial keratoplasty (EK). In this procedure the inner most layer of the cornea will be replaced by a similar healthy layer (like for like replacement). The decision upon which type of surgery is deemed appropriate is made by your doctor. This depends on the extent of the disease, type of the disease and the layers of the cornea involved.
After any of the above operations you will need to use long term steroid drops to keep the corneal immune system at bay. This will prevent the corneal graft rejection. However, sometimes the rejection can still happen despite this treatment.
Could I catch any disease from the transplant?
Before any organs can be used for transplant, the medical history of the donor is checked to exclude rabies, Creutzfeldt-Jakob disease (CJD) and certain other diseases of the nervous system.
Blood is taken from all donors to exclude hepatitis B, hepatitis C viruses and HIV.
The donor’s cornea is stored in the eye bank at the national transplant centre before being sent to the hospital where the operation is to be carried out. While the cornea is in the eye bank it is carefully examined to reduce the risk of infection with bacteria and fungi, therefore the risk of transmission of infection is tiny.
However, because of this tiny risk, once you have had a corneal transplant you will not be able to be a blood or organ donor.
What are the complications or risks?
As with all surgery there is a small risk involved. The complications of
corneal operations are rare, but can be very serious with potential life changing effects. So we are obliged to discuss these with you. Most complications of surgery can be managed successfully. All of these complications can lead to delay, require extra operations or treatment and extend the hospital stay.
Rejection of the corneal graft is the most common complication and occurs in about 1 in 7 patients at any time after the operation. It happens when your body detects a piece of tissue from another person and your immune system then tries to destroy it. Often it can be treated but sometimes a further corneal graft operation is required. Rejection of the graft is characterised by:
- Worsening of vision
- Redness
- Increased discomfort
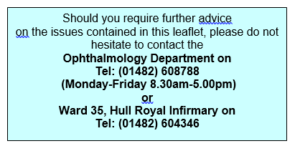
Should you have any concerns following your corneal graft in the future and are worried that you may be developing a graft rejection you should urgently contact the Eye Hospital at any time.
Minor complications can occur but do not usually affect the result:
- These include raised pressure in the eye or a leak of fluid between the stitches. Occasionally, if the leak does not seal on its own an extra stitch or replacement stitch is required.
Major complications are rare, but when they occur they can threaten the sight or even cause loss of the eye:
- When undertaking surgery to the front of the eye, bleeding can occur within the back half of the eye and this can lead to loss of sight.
- The normal process of the vitreous attachments to the retina becoming weakened as you age may be hastened by surgery on the eye. This process is called ‘posterior vitreous detachment’ and is normally characterised by flashes of light and floaters. In some people this process may cause holes to form in the retina causing a retinal detachment. If this occurs, then an additional operation may be required to repair this. This may happen several months after eye surgery.
- It is possible for the eye to develop an infection called endophthalmitis following surgery. Treatment for this type of infection involves further operation(s) to take samples and to allow injection of antibiotics into the eye. Treatment has to be very prompt if it is to be effective. 50% of cases of endophthalmitis do not recover sight, despite treatment. Very rarely does an eye have to be removed because of infection.
- Operations on one eye may produce an inflammation on the other eye (sympathetic ophthalmia). While this can usually be treated, it can result in loss of sight. This is an extremely rare complication of eye surgery and is more often described following eye injury (and even then is very rare).
- During local anaesthetic injections for eye surgery, it is possible for the eye to be punctured by the needle. This can lead to retinal detachment, bleeding or loss of vision. Local anaesthetic procedures can also cause bruising behind the eye. This can delay the surgery, or lead to loss of vision due to pressure on the eye nerve.
- Sometimes there is a higher than normal eye pressure following surgery. This may require the use of extra eye drops, pills or injections.
- Some patients may get bruising around the eye lids in the days following surgery. This type of bruising soon resolves.
How do I prepare for the operation?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination. Once you and your surgeon have agreed that you should have a corneal graft operation, you will be called to a pre-operative assessment clinic. At this appointment various tests will be performed to make sure that you are in good health for a general anaesthetic.
A corneal graft operation can be performed with the patient asleep (general anaesthetic), or the eye may just be numbed (local anaesthetic). This will be discussed with you.
You will be generally admitted to hospital on the day of your surgery, although in some circumstances you may need to be admitted the day before. This will be discussed with you.
Upon Arrival
The operation is carried out as an inpatient, you will be advised as to what time you need to be at the Eye Hospital on the day of surgery. You can expect to be in the hospital for at least 1 night.
Please report to the reception desk where you will be directed to the eye ward.
- Due to space restrictions, if you want to bring anyone with you, we request only one person accompanies you.
- Please bring a clean dressing gown and pair of slippers with you, with overnight clothing and toiletries.
- If you use a hearing aid, please also bring this with you.
- On the day of surgery, take your usual medications as normal, unless you have been advised to stop them prior to surgery.
- Also, please bring with you any medications that you may need to take whilst you are in hospital, including inhalers and sprays.
- Please do not wear any make up, nail varnish or jewellery, other than a wedding ring, as you will need to remove them before your operation.
- It is advisable not to bring valuables or money to the hospital, the Trust will not accept responsibility for loss or theft.
- Please eat and drink normally before coming in-to hospital, unless you have been advised not to do so.
- On arrival in the ward, a nurse will meet you and confirm the information that you gave at your pre-assessment appointment.
- We will give you eye drops before the operation. This is in order to dilate (widen) the pupil of the eye.
- You will be asked to get changed into a hospital gown and your dressing gown and slippers.
- Patients are offered drinks and light snacks free of charge.
- Visitors are asked to use the dining facilities in the main hospital or at the Women and Children’s Hospital. A drinks machine and some snacks are available on the ground floor of the Eye Hospital.
- During your stay several checks are made, these are to ensure that you will be receiving the correct treatment.
What actually takes place during the operation?
A routine corneal graft operation takes about 1 hour. If any other surgery is planned, such as cataract surgery, then it may take longer. This is only a guide as each patient is different.
During the operation, the surgeon removes a circular piece of your cornea and replaces it with a similar sized piece of the donor’s cornea, which is stitched into place. These stitches are not dissolvable and will need to be removed 1-2 years after the operation.
You will awaken with some soreness in the eye and the eye will be covered with an eye pad and plastic shield, which will be removed the day after surgery.
Patients undergoing Endothelial Keratoplasty (EK) will be requested to lie flat on their back after the surgery for a few hours. This helps the thin graft layer to attach to the inside of your cornea. Despite this some of these grafts do not attach the first time, and a small procedure may have to be performed in the first few days after the graft to correct this. This second procedure will also require you to lie flat on your back for several hours. You will be advised as to what to do accordingly by the medical and nursing staff team looking after you.
What happens afterwards?
Following the operation and after care:
Once you go home, it is important that you follow your post-operative instructions carefully. You will be told when you need to come for a check up, how to look after your eye and when to use the eye drops to help the eye to heal.
If you are worried about your corneal graft at any time then please contact the department for advice. The eye clinic has an open access policy for patients undergoing corneal graft surgery, so please do not feel that you are troubling people if there is a problem
Important points to remember:
- Wear your eye shield at night for as long as your surgeon recommends. You can expect to use it for two to three months.
- Use all eye drops as directed. If you have problems with any eye drops, contact the eye hospital. Do not discontinue or alter their use without checking with the surgeon first.
- Do not drive until you have your surgeon’s approval.
- Do not rub your eye.
- Avoid heavy lifting.
- Stay out of swimming pools and hot tubs for 3 months.
- Keep your eyes closed in the shower.
- Avoid dust, smoke (including cigarette smoke) and other eye irritants.
- You will need to be of work for 2 weeks following your surgery.
Long term recovery
- Following the surgery, the vision recovers over several months and is not instant. This is because the eye needs to recover.
- You will eventually need a sight test to see if glasses will help you see better.
- The final vision depends on the nature of the eye condition you had the surgery for. This will have been discussed with you prior to you going on the waiting list for surgery also when you sign the consent form for the operation.
- If you play sports, it is essential to wear eye protection at all times after a corneal graft
- You are strongly advised not to play major contact sports such as rugby, judo etc, at any time after a corneal graft, and not to recommence sports until you have been told that it is safe to do so.
- In the long term, a corneal graft is strong enough to stand the rigours of ordinary life, but an eye with a corneal graft is never as strong as a normal eye and may be split open by a severe blow such as a punch in the eye. Such an injury can cause blindness.
This leaflet was produced by the Ophthalmology Department, Hull University Teaching Hospitals NHS Trust and will be reviewed in May 2026.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.
Your newborn baby’s NHS number
An NHS number is allocated to everyone whose birth is registered with a Registrar of Births and Deaths in England and Wales. You already have an NHS number and your baby will be assigned an NHS number soon after birth. Your NHS number is unique to you and provides a reliable means of linking you to the medical and administrative information we hold about you. NHS numbers are allocated on a random basis and, in themselves, provide no information about the people to whom they relate.

