- Reference Number: HEY1247/2021
- Departments: Speech and Language
- Last Updated: 31 August 2021
Introduction
This advice sheet has been produced to give you information about eating and drinking when there is a risk of aspiration. It is not meant to replace discussion between you and your doctor and / or speech and language therapist. If after reading it, you require further explanation please discuss this with the relevant person who has been caring for you.
Eating and drinking and risk of aspiration
If you are experiencing swallowing problems, there may be a risk of food, fluids or saliva ‘going down the wrong way’ – into the windpipe and the lungs. This is known as aspiration.
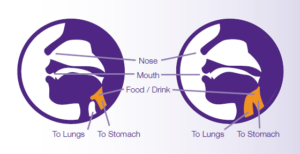
Diagram courtesy of Nutricia
Signs of swallowing difficulties include:
- Food collecting in the mouth
- Coughing or throat clearing
- Choking
- A wet, ‘gurgly’ voice
- Difficulty breathing and/or noisy breathing
- Shortness of breath after eating and drinking
- Feeling the food or drink ‘going down the wrong way’
Some people with swallowing difficulties may aspirate without showing any of the above signs. This is known as silent aspiration.
People who aspirate may develop recurrent chest infections and, in some cases, this could be fatal. Malnutrition and dehydration are also closely linked with dysphagia.
If you have been diagnosed with a swallowing difficulty which places you at risk of aspiration and a feeding tube is not suitable for you (or you have declined this as an option), it may be appropriate to continue to eat and drink acknowledging the risks. This is known as ‘eating and drinking for quality of life’.
Eating and drinking for quality of life may be appropriate for one or more of the following reasons:
- Advanced stage of illness
- The person’s swallow safety is unlikely to improve
- The preference to eat and drink takes priority over swallow safety
- Tube feeding options are inappropriate or declined
It is important that all the advantages and disadvantages of eating and drinking with risk have been discussed with you so that you are able to make an informed choice regarding this. If you are unable to make the decision yourself, the decision will be made by the medical team or your health care power of attorney during a best interest meeting.
This meeting will involve your family or carers so that they are able to inform us of any discussions you may have had regarding this. The decision will be made and clearly communicated to your family and carers. Discussion will also include advanced care planning including decisions regarding treatment options for aspiration related chest infections, pneumonias, readmissions to hospital and referral to palliative services.
The emphasis when eating and drinking for quality of life is on maintaining optimum comfort. Certain symptoms of an unsafe swallow such as choking and violent coughing may cause undue distress and negatively impact quality of life. If these symptoms occur, it may be appropriate to stop eating and drinking and focus on maintaining good oral hygiene and using flavoured swabs for taste.
You will be provided with a document called ‘Passport for those Eating and Drinking for Quality of Life’ which will outline your decisions and choices.
What can help when you are eating and drinking with risk?
Your Speech and Language Therapist can advise on particular consistencies of food or fluids which may reduce, but not eliminate the risk of aspiration. Patient comfort will always be a priority when making these recommendations.
Sensible precautions when eating and drinking include:
- You must be sitting upright, and be alert.
- Assistance and supervision as required.
- Take small mouthfuls.
- Be aware your appetite may be smaller than normal.
- Smaller, more frequent meals or snacks and drinks may be easier.
- Take plenty of time for each mouthful to be swallowed.
- Avoid the use of straws and spouted cups unless advised, as these may increase risk of choking.
- It is important to have foods and drinks you enjoy but remember the advice you have been given about the safest and most comfortable consistencies – this may also relate to any supplements that the dietitian has prescribed for you.
Oral hygiene
It is important to maintain a clean and healthy mouth. A build-up of bacteria can also be aspirated into the lungs and can lead to increased risk of chest infections.
Contact Details:
If you would like to discuss the information on this advice sheet further, please speak to your doctor or Speech & Language Therapist. Speech & Language Therapy Department: Hull Royal Infirmary tel: 01482 604331 or Castle Hill Hospital tel: 01482 875875 Extension:3155

