- Reference Number: HEY1523/2025
- Departments: Endoscopy
- Last Updated: 31 March 2025
Introduction
This leaflet has been produced to give you some information about your Endoscopic Ultrasound (EUS) procedure. Most of your questions will be answered by this leaflet, but it’s not intended to replace the discussion between you and your consultant. If after reading this leaflet you have any questions or require further explanation, please contact a member of the healthcare team.
Endoscopy Department, Castle Hill Hospital, contact number: tel: 01482 622069 (direct line)
What is Endoscopic Ultrasound?
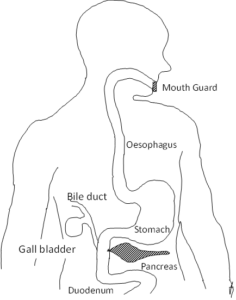
Endoscopic ultrasound (EUS) is an internal examination carried out with a slim flexible tube (endoscope) with a video camera and an ultrasound probe on the end which allows a trained specialist to look directly at your gullet (oesophagus), stomach, and first part of the small intestine (duodenum), and using ultrasound, also look at the organs inside your chest and abdomen. Pictures from inside your chest and abdomen are examined on a video monitor and an ultrasound monitor. A small sample of tissue (biopsy) may in some cases be taken painlessly during the procedure for analysis in the laboratory, using the camera and the ultrasound to direct the instrument for the biopsy.
This diagram shows the route taken by the Endoscopic Ultrasound (EUS) instrument from the mouth, down the oesophagus, into the stomach and then into the duodenum where it is able to inspect for abnormalities in the pancreas, the bile duct, lymph glands and many other areas.
Why do I need Endoscopic Ultrasound?
Endoscopic Ultrasound (EUS) is needed by your hospital consultant as part of your investigations and / or treatment, and it is often arranged as part of a number of other tests and scans, to add to the information about your condition, so that your treatment can be tailored to your individual needs. It is a procedure that is arranged after detailed consideration of many factors and often after discussion between several members of the clinical team looking after you.
In case you are wondering why you need to travel a long distance for this procedure, EUS is a highly technical test and is only available in some hospitals, and in this region, this is Castle Hill Hospital.
Does Endoscopic Ultrasound have any side effects or complications?
Endoscopic Ultrasound (EUS) is a safe procedure. We will make every effort to make sure that you are as comfortable and as safe as possible. Side effects, which are not serious and tend to settle without treatment, include slight bruising at the site of the cannula (which is inserted into a vein in your arm or the back of your hand to give you a sedative), a sore throat and possibly bloating.
EUS carries a very small risk of complications, these include haemorrhage (bleeding) or perforation (a tear or hole) of the oesophagus or stomach or duodenum. If one of these rare complications occurs, you will need to be admitted to hospital as a precaution; and in a few cases an operation is needed to repair any damage.
Sedatives are given through a cannula inserted into a vein just before the EUS procedure. Very rarely allergic reactions to the sedatives can occur. A few people are particularly sensitive to sedatives, but the effects will be monitored throughout the procedure and for a period of time afterwards in the recovery area of the Endoscopy Department. If there is any concern during the EUS procedure it will be stopped promptly, and if required, an antidote which reverses the effect of the sedation will be given. This is usually all that is needed and recovery is swift and complete with no lasting adverse effects.
In some cases, particularly in people who have another medical condition (e.g. heart disease, unstable angina, stroke, severe asthma or chronic bronchitis) the sedative drugs can cause difficulty with breathing. This is rare and every patient is given oxygen (through a small tube under the nose) during the procedure and their breathing and pulse rate monitored throughout. Aspiration pneumonia (fluid inhaled into the lungs) is a very rare complication of any endoscopy procedure including EUS and one that we do our best to guard against. There is a slight risk of damage to crowned teeth or dental bridgework.
All patients where any of these rare events occur, will be informed of their occurrence as part of the NHS duty of candour regulations. If you would like to know more about any of these issues, please ask your nurse or specialist about the hospitals complication rate.
Are there alternatives to Endoscopic Ultrasound?
Endoscopic Ultrasound (EUS) is a unique procedure and often adds valuable information about your condition that is not obtainable by any other test or scan. Without EUS some vital information about your condition may be lacking or absent altogether.
What happens if I refuse to have Endoscopic Ultrasound?
You are entitled to decline to have Endoscopic Ultrasound (EUS). This will not alter the way in which you are treated. However, it will mean that there will be important or even vital pieces of information that will be absent when making plans for your treatment. EUS is a procedure that is arranged after a great deal of consideration and requires significant planning and NHS resources.
Please don’t simply not turn up for your EUS appointment. Discuss your decision with your consultant or their team first. If you still don’t wish to have the procedure then please let us know in good time (direct line tel: 01482 622069), so that we can reallocate the appointment to another patient on the waiting list, who may have a serious condition; help to save valuable NHS resources.
Will I need Endoscopic Ultrasound again?
This will depend on the reason for the Endoscopic Ultrasound (EUS) in the first place, and on what is found during the EUS and whether it is possible to complete everything that’s required. Your nurse or your specialist will keep you informed of any further appointments.
Who will do the Endoscopic Ultrasound?
It will be a specialist consultant who is highly trained and experienced in performing Endoscopic Ultrasound (EUS). Occasionally another consultant or very senior doctor who is undertaking advanced training in EUS may perform your procedure under close supervision by an EUS specialist, but you will always be informed, and your permission will be obtained in advance for this, and the quality of the procedure is never compromised. You can choose to have the specialist carry out your procedure.
Where will the Endoscopic Ultrasound be performed?
Endoscopic Ultrasound (EUS) is performed in the Endoscopy Department at Castle Hill Hospital. Directions will be given with your appointment letter. You will need to make sure that you attend in good time for your appointment, allowing for traffic conditions and time for onsite parking (if travelling by car).
How do I prepare for my Endoscopic Ultrasound procedure?
Read this information leaflet fully. Share the information it contains with your partner and family (if you wish) so that they can help and support you. There may be information they need to know, especially if they are taking care of you once you have had the Endoscopic Ultrasound (EUS) examination. Complete any health questionnaire sent/given to you as fully as possible.
Your stomach needs to be empty so that EUS can get a clear view. You should not have anything to eat or drink for at least 6 to 8 hours before your test (and longer if this is what you have been advised) except for small sips of water (but not any other drinks) up to 3 hours before the test, to keep yourself hydrated.
Take any regular medicines that you normally take as usual. It is however important for us to know well before the day of your appointment if you are on certain medicines or tablets, these are:
- WARFARIN – or any other blood thinning treatment, such as RIVAROXABAN, APIXABAN, DABIGATRAN, ARGATROBAN, EDOXABAN which may have to be stopped for a period of time before your test.
- CLOPIDOGREL (PLAVIX) – or any other anti-platelet tablets which may need to be temporarily stopped before your test.
You must contact the Endoscopy Department at Castle Hill Hospital for advice well before the date of your appointment if you are taking any of the treatments listed above.
If you have diabetes (especially if you normally have insulin) or you have serious heart, lung or kidney problems, or are concerned that a health problem you have may be affected, then contact the Endoscopy Department at Castle Hill Hospital.
- PREGNANCY – It’s important that you inform us if there is any possibility that you may be pregnant. Any information you share with us will be kept strictly confidential.
- LATEX ALLERGY – Inform the Endoscopy Department if you have a confirmed latex allergy as this will influence your appointment time, in order to minimise any risk to you.
- CJD (Creutzfeldt-Jakob disease/ variant Creutzfeldt-Jakob disease) – Inform the Endoscopy Department if you have been notified that you are at risk of CJD/ vCJD by any public health individual or organisation.
What happens to me in the Endoscopy Department?
Our reception staff will greet you on arrival and will let a nurse know that you have arrived. A nurse will collect you from the waiting room and explain what will happen next. You will be given an approximate time of when you may be ready to be collected to go home after your procedure. You are advised to leave any valuables at home.
The nurse will escort you to a private assessment room and ask you questions about your general health and go through the health questionnaire that you completed for us. The nurse will check your blood pressure, pulse, and oxygen levels. A nurse may carry out a finger prick blood test (called an INR test) in some cases. If you are having sedation, a cannula will be inserted into a vein in the back of your hand or in your arm. No sedation is given at this stage.
The specialist doing the procedure will meet you and explain the details of the Endoscopic Ultrasound (EUS) test to you and explain if a biopsy is going to be carried out. You will both sign a consent form. This is to show that you understand the information that you have been given and agree to the procedure being performed. At any point before or during the procedure you can withdraw your consent; if this happens the specialist will stop the test.
You may have a short wait for your procedure in a waiting area, and we will do our best to carry out your procedure as close to the specified time as possible, but occasionally there may be a delay in your appointment time due to technical requirements or cleaning routines or an emergency taking priority ahead of you. If there is a delay, you will be notified as soon as possible and kept updated.
When your EUS procedure is due, you will be escorted to the examination room where you will be made comfortable on a bed or trolley. If you wear glasses or dentures, you will be asked to remove them. A final safety check will be carried out to confirm your name, date of birth and the procedure you are having. You will be asked to turn onto your left side. To protect your teeth/ gums (and our EUS instrument), a plastic mouth guard will be placed between your teeth/gums. A fine plastic tube will rest under your nose to give you some extra oxygen. A soft peg will be placed on your finger to monitor your oxygen levels and pulse rate. If you are having sedation, it will be given at this time, and you will feel sleepy and lightheaded.
Do I need sedation?
Most patients have a local anaesthetic spray first, to numb the back of the throat. This is not a sedative. The sedative itself is given through a cannula inserted into a vein in the back of your hand or in your arm and is given just before the procedure. This will make you sleepy and relaxed and make you comfortable during the procedure. It is not a general anaesthetic and does not put you completely to sleep. The specialist may also give you pain relief medication also through the cannula before the test begins, depending on the type of Endoscopic Ultrasound (EUS) that you are having.
Do I really need someone with me after sedation?
It is essential that you have someone with you if you have had sedation. The sedation you are given can have effects which last for up to 24 hours after the procedure. You can become forgetful and also sleepy again. Your procedure may be cancelled if you do not arrange to have someone collect you and stay with you for the full 24 hours.
We strongly recommend that for 24 hours you after sedation that you:
- Do not drive or operate machinery
- Do not return to work
- Do not sign any important / legal documents
- Are not left alone, as you may be at risk of injuring yourself
- Are not left alone to care for children.
If you are an outpatient, the person accompanying you will be contacted to collect you.
If you are an inpatient at Castle Hill Hospital, you will be transferred back to your ward.
If you are an inpatient at another hospital (not Castle Hill Hospital), you will be transferred back to your hospital on the same day.
If you have been told that you will be admitted to Castle Hill Hospital after the procedure (for example patients having an Axios stent fitted) you will remain in the Endoscopy Department until you are transferred to a ward.
What does having Endoscopic Ultrasound feel like?
Once you have had the sedation you may be very sleepy and unaware of the examination until it is completed. However, in some cases, you may be just very drowsy and aware of the flexible instrument going over your tongue to the back of your throat. It will not interfere with your breathing, and any initial gagging or retching settles quickly, and any saliva is cleared for you with a sucker. Some air may be passed down the instrument to inflate your stomach and allow a clear view.
How can I help myself?
A nurse will be sitting by your head all through the procedure and you can help by listening to the instructions your nurse gives you. If you are not asleep and just drowsy then close your eyes, stay calm and relaxed, and adopt a regular slow deep breathing pattern, through your nose or through your mouth, this often adds to the relaxation and improves the experience. The nurse and specialist will be aware that you are not asleep and will talk to you, explain and reassure you, and help you adopt the correct breathing pattern during the procedure.
What happens when at the end of the test?
The test takes on average 30-40 minutes. It can take longer; in which case you will receive a top up of the sedation. If you have had sedation, you will need to rest on a trolley in the recovery room for approximately 30-60 minutes. If you have had a biopsy, then you will be observed for longer. You will be helped to a chair and given a drink. It is quite likely that the back of your throat will feel sore, and you may feel a little bloated, but these will settle without any medication.
When do I get the results?
The findings from your test will need careful analysis and the results will not be available immediately. A report will be sent to your consultant. The nurse in the recovery area will check that you have a follow-up appointment with your own consultant before you leave the department. This will be written on your discharge form with any instructions that you need to follow.
Do you need further information?
If you require further information about your test, then your consultant, or alternatively the Endoscopy Department at Castle Hill Hospital are valuable sources for information.
Further information about your rights with regards to consent can be found in the following documents: These are free of charge.
- Department of Health (2001), Guide to Consent for Examination or Treatment.
- Department of Health (2001), Consent – What you have a right to expect.
- A Guide for Adults. (Available from the Endoscopy Department)
- A Guide for Relatives and Carers. (Available from the Endoscopy Department)
Visit the Department of Health’s website at: www.doh.gov.uk and for consent: www.doh.gov.uk/consent
Useful contact numbers:
Main Contact: The Endoscopy Department, Castle Hill Hospital tel: 01482 622069 (direct line) Monday to Friday: 8.00am to 5.00pm
Other contacts:
Endoscopy Department, Hull Royal Infirmary tel: 01482 674790 Monday to Friday: 8.00am to 5.00pm.
Ward 100, Hull Royal Infirmary Out of hours tel: 01482 674860
What do the words in the leaflet mean?
- Biopsy: a sample of tissue taken during Endoscopic Ultrasound (EUS) for close examination in the laboratory under a microscope. The result can take 10 to 14days to be available.
- Consent: a signed agreement between you and the specialist doing your EUS procedure, confirming that you understand the information about the test particularly the reason for the test, and the risks, and that you agree to proceed with it.
- Duodenum: The part of the gut leading from the stomach
- Endoscopy Department: the place where the EUS is done
- Endoscope: a tube for looking inside the body. EUS is done with a special type of endoscope that has both a miniature video camera and an ultrasound probe on its tip.
- Oesophagus: the gullet leading from the mouth to the stomach
- Specialist: the consultant specialising in EUS who will be doing your procedure or who will be closely supervising a qualified doctor training in EUS.
- INR: the test carried out to check that the natural bloods clotting ability is safe for a biopsy
General Advice and Consent
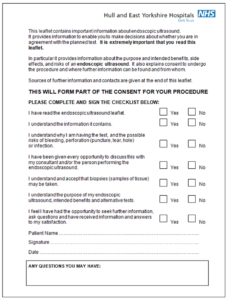
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

