- Reference Number: HEY212-2024
- Departments: Endoscopy
- Last Updated: 3 June 2024
Introduction
This leaflet has been produced to give you general information about your procedure. Most of your questions should have been answered by this leaflet. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team who has been caring for you.
What is an ERCP?
Endoscopic Retrograde Cholangiopancreatography) (ERCP) is a procedure where a flexible tube with a camera on the end is passed through the mouth into the first part of the small bowel. The opening to the bile and pancreatic ducts can be seen. A flexible wire is passed down the endoscope into the opening. Dye is then injected which is shown up on the X-ray to confirm the position of the equipment and bile duct.
ERCP and sphincterotomy
If the X-rays confirmed a stone is blocking the bile duct, the doctor will widen the opening of the bile duct by making a small cut called a sphincterotomy. We aim to clear the bile duct of stones that will later pass out through the digestive tract.
ERCP and stent replacement
If the X-rays show a blockage in the bile duct, or if doctor is unable to clear the duct of the stones, the doctor may place a small plastic or metal tube (stent) into the duct. This allows bile to drain into the intestine again. If you have had jaundice, this will relieve the jaundice and your itching. Plastic tubes can be removed or replaced at a later date if necessary through a similar procedure.
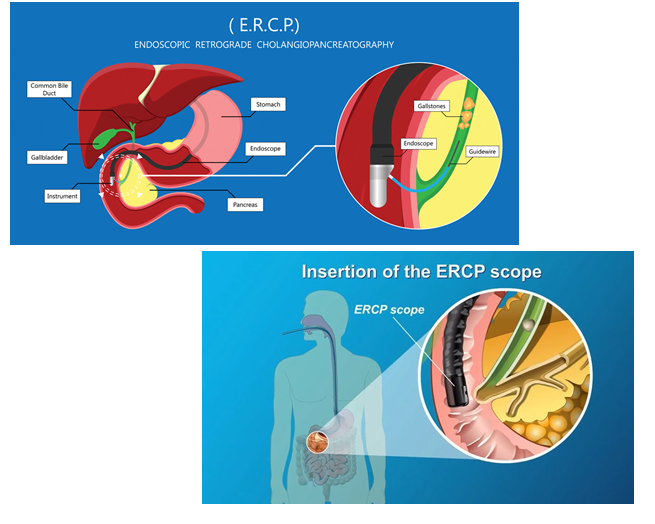
The basics of the procedure is illustrated as follows:
Why do I need an ERCP?
Your doctor may recommend the procedure if you have a blockage in the bile flow which may cause symptoms of jaundice with or without tummy pain, fever, weight loss, pale stools or loss of appetite.
Can there be any complications or risks?
All medical procedures carry some element of risk. These will be discussed with you before the procedure where you will be given the opportunity to ask any questions or raise any concerns you may have.
Possible complications:
- Pain: Any pain you experience will be monitored by the nurse looking after you. Analgesia (painkillers) can be administered as required.
- Sedation: The sedation we use is a conscious sedation. People have sedation to keep them comfortable while the doctor carries out the test. Sedation is given through a cannula in the back of your hand. It makes you feel sleepy and relaxed but does not put you to sleep. You can still respond to what is happening and may feel dazed. However, even with conscious sedation it maybe poorly tolerated, thus you may need increased sedation.
- Teeth or Bridgework Damage: Rarely, the equipment might damage teeth. A mouthguard is used to lower this risk. If you have loose teeth, please discuss this with your endoscopist prior to the procedure.
- Procedure Failure: Sometimes, the procedure might not find or treat the problem. This can happen if the duct is hard to reach or if a stone cannot be removed. There may also be a failure to place the stent in the correct position in minority of cases.
- Pancreatitis: Inflammation of the pancreas can happen in about 4 to 6% of cases within a day or two. To reduce the risk of this, a medication (anti-inflammatory) is inserted into your back passage (suppository ) prior to the procedure. Rarely it can be severe enough to require admission to the intensive care unit for treatment.
- Bleeding: Bleeding might occur during or after the procedure in about 6% of cases, especially if you are on blood-thinning medications.
- Perforation: Rarely, the equipment or catheters might make a hole in the organs being examined. This may need surgery to fix.
- Bile Duct Infection: Infection of the bile ducts is rare but serious. Antibiotics are sometimes given before the procedure to lower this risk and in some cases a course is given if there are signs of infection.
- Aspiration: Sometimes, food can go into the lungs while you are sedated, causing infection. Antibiotics and treatment can help if this happens.
- Death: Very rarely, death can occur due to complications as above rather than from the procedure itself, especially in older people, emergency cases, or those with serious illnesses.
Possible long term complications:
- Stent Movement: If a small tube is placed in the bile duct, it might move and need to be removed with repeat procedure.
- Stricture: Though uncommon, bile duct narrowing can happen over time after sphincterotomy, restricting bile flow. This might need more treatment via stents.
Other things to know:
- Sensitivity to Sedation: Some people might react strongly to sedation. If this happens, we can stop the procedure and give an antidote. This is rare and is why we monitor your vitals throughout; and why we give oxygen by nasal tubes.
- Risks Vary: Complications depend on factors like your health, the reason for the test, and what’s found during the procedure. Your doctor will talk to you about the risks before the test.
How do I prepare for the ERCP?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination. Complete the health questionnaire sent/given to you as fully as possible.
How long will I be in hospital?
You will usually be in the hospital for about 3 hours. Sometimes, if you are at higher risk or unexpected things come up, you might need to stay overnight. They will let you know in your appointment letter. However, it is best to bring a small overnight bag with you.
Before Your Procedure:
- Empty Stomach: To see things clearly, your stomach and the start of your intestine should be empty. Do not eat or drink anything for at least 6 hours before your test.
- Special Health Conditions: If you have diabetes, serious heart, lung, or kidney problems, or concerned that a health problem you have may be affected, let the Endoscopy Department know. You will find their contact numbers at the top.
- If you are allergic to latex or have been told you might be at risk for Creutzfeldt-Jakob disease (also known as mad cow disease). Please inform the department if you have been notified that you are at risk of CJD/vCJD for public health reasons.
- Pregnancy: If you could be pregnant, it’s really important to tell us. Any information you share with us will be kept strictly confidential.
- Medications: If you take certain medications, like blood thinners, insulin there are specific instructions. Contact the Endoscopy Department for advice.
- Blood Thinners: If you take certain blood thinning medications like Warfarin, Apixaban, Rivaroxaban, Dabigatran, Argatroban, Or Edoxaban or Clopidogrel, get in touch with the Endoscopy Department before your appointment. They might need to be stopped for a period of days before the procedure to lower the risk of bleeding.
Remember, your safety and comfort are important, so make sure to follow these instructions.
What happens to me in the Endoscopy Department?
Our welcoming reception team will greet you when you arrive. If there is a delay due to an emergency, we will inform you promptly.
A nurse will guide you from the waiting room, explain the next steps, and give you an estimated time for when you can be collected to go home. It is best to leave valuables at home.
We will ask about your health and go through the questionnaire you filled out. Feel free to ask any questions.
The doctor doing the procedure will meet you, explain it, and you will both sign a consent form. You can stop the procedure anytime by withdrawing your consent. Let us know if you are unsure or worried.
You might need a blood test before or on the procedure day. Any urgent abnormality would need to be treated prior to the procedure taking place. For some safety reasons, the procedure may need to be rescheduled.
If needed, antibiotics might be given. We will check your vital signs before, during, and after the test. Glasses or dentures should be removed.
In the examination room, you will lie on your left side. X-ray and endoscopy equipment will be around, and staff will wear protective gear. The amount of x-rays you receive are strictly controlled.
If you are having sedation, you will get it now and feel sleepy but not completely asleep .
To help your breathing, we will give you a bit of oxygen through your nose.
A mouth guard keeps your mouth open. Sometimes diathermy (gently cutting with an electrically heated wire) will be used internally in the gut. A special pad will be placed on your leg for safety.
The test usually takes about 30 minutes.
Do I need sedation?
Yes. People have sedation to keep them comfortable while the doctor carries out the test. Sedation is given through a cannula in the back of your hand. It makes you feel sleepy and relaxed but does not put you to sleep. You can still respond to what is happening and may feel dazed. However, even with conscious sedation it maybe poorly tolerated, thus you may need increased sedation.
Do I really need someone with me after sedation?
Yes, this is very important as sedation can have side-effects, which last some 24 hours after the test. You can become forgetful and also sleepy again. Your test may be cancelled if you do not arrange to have someone to collect you and stay with you for the next 24 hours.
We strongly recommend that for the next 24 hours you:
- Do not drive
- Do not return to work or operate machinery
- Do not sign any important/or legal documents
- Are not left alone, you may be at risk of injuring yourself
- Are not left alone to care for children
If you are an outpatient, the person accompanying you will be contacted to collect you. If you are an inpatient you will be transferred back to your ward.
What will the test feel like?
You may feel the tube gently slide over your tongue and down your gullet. It will not be painful, or interfere with your breathing. If you get a lot of saliva a nurse will use a suction tool. You may feel nausea and retching as the tube passes from the back of your throat, this will pass and try to relax. You may feel the tube move around in your stomach. Some air will be passed down the tube to inflate your stomach and first part of small intestine to allow a clear view.
A non-steroidal anti-inflammatory medication would be inserted in your back-passage prior to your procedure. This is to prevent the complications of Post ERCP pancreatitis. Please advise the doctor if you DO NOT consent to this.
How can I help myself?
You can help by listening to the instructions your nurse gives you. By staying calm and relaxed, the test goes quickly and easily. Try to control your breathing by taking slow deep breaths. This helps stop you wanting to retch.
What happens when the Procedure is finished?
When the ERCP is finished, you will be transferred to the recovery room to rest for about an hour. When you have recovered, you will be helped to a chair and given a drink. Please take care because the sedative may make you feel dizzy and a little confused when you get off the examination trolley.
It is for these reasons that, when you have sedation, someone should bring you and take you home. If you live alone, contact the Endoscopy Department so we can arrange help.
It is quite likely that the back of your throat will feel sore for the rest of the day.
You may feel bloated if some air remains in your stomach. Both discomforts usually pass without any medication; you may find it helpful to eat light meals for the next 24 hours.
The immediate/early complications are pain in your tummy, perforation, bleeding and aspiration. The delayed complications are including above and those highlighted earlier which may need hospital admission and treatment.
When do I get the results?
The Recovery nurse will explain your test results to you and (if you wish) the results will be told to your carer. These will be written on your discharge form with any instructions that you need to follow. Your own doctor and hospital doctor will receive a copy of the results.
Will I ever need an ERCP again?
This will depend on the reason for the ERCP, what is found and whether it was possible to complete the test.
It may be necessary to repeat the test after a few weeks, if stones have been not fully removed or to check the ducts are clear.
If it was necessary to insert a stent (tube) into the duct during the test, it may need to be changed or removed after some time.
Your nurse will keep you informed of any further appointments.
Further information
If you require further information about your test your GP, consultant, and the Endoscopy Department is a valuable source of information.
Further information about your rights with regards to consent can be found in the following documents.
- Department of Health (2001), Guide to Consent for Examination or Treatment.
- Department of Health (2001), Consent – What you have a right to expect.
- A Guide for Adults. (Available from the Endoscopy Department)
- A Guide for Relatives and Carers. (Available from the Endoscopy Department)
These are free of charge.
Visit the Department of Health’s website at: www.doh.gov.uk and for consent: www.doh.gov.uk/consent
Useful contact numbers:
The Endoscopy Department, Castle Hill Hospital, tel: 01482 622069 (direct line) Monday to Friday from 8.00 am to 5.00 pm
The Endoscopy Department, Hull Royal Infirmary, tel: 01482 674790, Monday to Friday from 8.00 am to 5.00 pm
Ward 100 Hull Royal Infirmary Out of hours, tel: 01482 674860
What do the words in the leaflet mean?
- Bile: A fluid produced in the liver and passed into the gut via the bile ducts.
- Biopsy: A sample of tissue is taken for analysis.
- Consent: This is the agreement between you and the endoscopist. You are agreeing to have investigations or treatment and that you understand the purpose, benefits, alternatives and risks. You and the endoscopist during this process usually sign a consent form.
- Duodenum: The part of the gut leading from the stomach.
- Endoscopy Department: The place where your procedure takes place.
- Endoscope: A tube for looking inside the body.
- Endoscopist: This can either be your consultant, an experienced and trained doctor or an experienced and specially trained practitioner.
- ERCP: Endoscopic Retrograde Cholangiopancreatography.
- Gall Stones: Stones usually formed from crystals of cholesterol in the gall bladder.
- Oesophagus: The gullet. The pipe leading from the mouth to the stomach.
- Pancreas: Gland which delivers enzymes into the duodemum for the digestion of food.
- Pancreatitis: Inflammation of the pancreas.
- Stent: A plastic or metal tube inserted in your bile or pancreatic duct.
- Sphincter: A muscular valve.
- Sphincterotomy: Cutting an opening into the bile duct.
- Stricture: Narrowing.
- Therapeutic: Something done or given that will treat illness.
This leaflet has been written with the help, support, advice and collaboration of:
- Consultants of the Department of Gastroenterology
- Consultants of the Surgical Department
- Staff of the Endoscopy Department
- Patients attending the Endoscopy Department
Endoscopy Department contact numbers:
Hull Royal Infirmary, tel: 01482 674790 (direct line)
Castle Hill Hospital, tel: 01482 622069 (direct line)
You will be given an Oesophageal Dilatation Information Checklist to complete as part of the consent for your procedure – please see the link:
HEY212-2024_Endoscopic Retrograde Cholangiopancreatography (ERCP Consent form word

