- Reference Number: HEY1372/2023
- Departments: Paediatrics, Physiotherapy, Therapies
- Last Updated: 31 August 2023
Introduction
This leaflet has been produced to give you general information. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a Patient-Initiated Follow-Up (PIFU) pathway?
A patient-initiated follow-up (PIFU) means that we will not routinely book you an appointment, instead we are putting you in control of making your own appointments at a time when you need them most, within a given timeframe.
How does PIFU work?
You will have been given this leaflet because your healthcare professional is happy that you do not need to see them again unless you have a problem. If you do have any problems, you can contact the Paediatric Therapy department on the given telephone number and they will arrange an appointment, either by telephone or face-to-face if it is needed. You will be told how long after your injury that you can contact the Paediatric Therapy department, on the PIFU pathway if you need to be seen.
When should I call for a PIFU?
You can call to make an appointment if you
- are not improving to a level that was expected
- have worsening symptoms relating to your injury/condition
- have a “flare-up”
Please note, you can only initiate a PIFU appointment for the specific injury/condition you were originally referred to the Paediatric Therapy service for.
When should I not use PIFU?
- If your concern is related to different injury/condition
- If the specified time period has lapsed, please contact your GP.
- If you need urgent medical advice you should contact your GP or NHS111.
What if I don’t need a PIFU follow-up appointment?
You do not have to arrange an appointment if you feel it is not required. If you don’t contact us to book an appointment within the specified timeframe, the PIFU will expire and you will be discharged back to the care of your GP. We will not contact you to book a PIFU appointment – it must be initiated by you.
What is a finger and thumb interphalangeal (IP) joint dislocation or thumb metacarpal (MCP) joint dislocation?
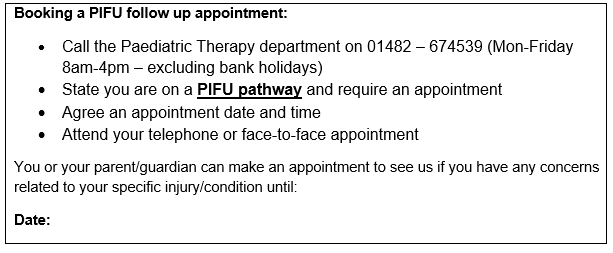
The finger and thumb interphalangeal (IP) joints are the small joints of the fingers and thumb. They are the joints between the finger bones. There are two interphalangeal (IP) joints in each finger, the proximal interphalangeal joint (PIPjt) and the distal interphalangeal joint (DIPjt). There is one interphalangeal joint in the thumb (IPjt). The thumb metacarpal joint (1st MCPjt) is the joint between the thumb bone and the hand bone.
A dislocation of these joints is when there is an abnormal separation of the two gliding surfaces. If the joint surfaces are only partly separated this is called a subluxation. An associated small fracture (avulsion) of the adjacent bones is quite common.
How should it be treated?
Any dislocated or subluxed joint needs to be put back in place as soon as possible (reduced). This is sometimes done immediately if there is someone present who can perform the procedure. More frequently it will be done in the local Accident and Emergency department.
If the joint is reduced quickly and the joint is stable, good recovery can be expected. The finger may be temporarily strapped to the adjacent finger to provide support but should not prevent movement. The tape should be applied in thin strips above and below the affected joint. This tape should be removed, the hand washed and reapplied on a daily basis. Tape should be discarded completely at 3 weeks.
What should I do in the first few days?
The affected joint will be swollen and stiff. It is important to gently and regularly move the joint. Complete rest is not advisable. It is important that you try to use your hand normally when doing everyday tasks such as washing, dressing and eating.
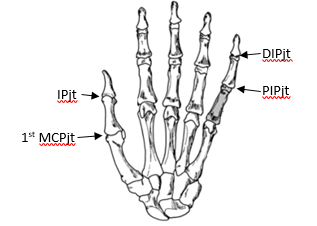
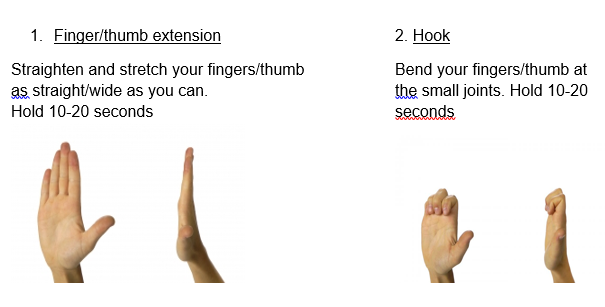
Exercising the finger or thumb early is very important to prevent stiffness. The following exercises should each be repeated 10 times and completed every 2-3 hours. Support your elbow on the table with your wrist straight.
Swelling
Swelling is a normal reaction following joint dislocation and can take several months to settle fully. It is important to minimise this as much as possible by doing the following:
- Elevate the hand, especially at night on pillows.
- Ice – massage with an ice cube. Remembering to keep it moving.
- Massage along the finger or thumb towards the wrist.
- Complete the exercises above
What about play and school?
You can use your hand for light daily activities such as eating, dressing and light school activities as soon as you feel comfortable. Carrying heavy bags or attending PE at school is best avoided until 6 weeks after your injury.
Full contact sport should also be avoided for at least 6 weeks and until you have full range of movement and strength. You should start by practicing sports specific activities; like throwing or catching. Build up these activities gradually from around 6 weeks in order to regain strength and flexibility before returning to full training sessions and competition.
Possible complications and when to initiate PIFU?
Joint stiffness and a flexion contracture (the joint remaining in a bent position) are the most common complications. These can be avoided by following the above information regarding minimising swelling and encouraging movement. However, on occasion this will still develop.
Please initiate a Patient Initiated Follow UP (PIFU) appointment if
- You are struggling to fully straighten your finger or thumb at 3 weeks following your injury or you feel it is getting worse
- You are struggling to make a full fist or reach the base of your little finger with your thumb tip at 3 weeks following your injury
- You feel your movement or function is worsening
- Your pain or swelling worsens
- You are struggling to return to your daily activities or hobbies after 6 weeks.
If we do not hear from you 3 months following your injury date we will assume that you no longer require any further intervention and will be discharged from the PIFU pathway. If you have further problems with your finger after this date please contact your GP practice.
Should you require further advice on the issues contained in this leaflet or wish to initiate a PIFU appointment, please do not hesitate to contact the Paediatric Therapy Department on telephone: 01482 674539.
This leaflet was produced by the Paediatric Therapy Team, Hull University Teaching Hospitals NHS Trust and will be reviewed in August 2026
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats your child, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to your child. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your child’s condition, the alternatives available for your child, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about your child
We collect and use your child’s information to provide your child with care and treatment. As part of your child’s care, information about your child will be shared between members of a healthcare team, some of whom you may not meet. Your child’s information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide your child with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your child’s doctor, or the person caring for your child.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about your child. For further information visit the following page: Confidential Information about You.
If you need information about your child’s (or a child you care for) health and wellbeing and their care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

