- Reference Number: HEY1306/2022
- Departments:
- Last Updated: 31 May 2022
BREAST CARE UNIT – Information for Patients
Introduction
This leaflet explains about going home with a Redivac drain following Breast Surgery. Most of your questions should be answered by this leaflet. If after reading it you have any concerns or require further explanation, please discuss this with the Nurse caring for you on the ward or your Doctor.
Why do I need a drain?
Following surgery to the breast or axilla a drain may be inserted. The drain will help to prevent a build-up of fluid (seroma) from forming and causing swelling and discomfort. The drain will also minimise any bruising to the area.
The drain will normally stay in situ approximately for 3-10 days, this may need to be longer depending upon how much fluid is draining each day and the type of surgery you have had. We advise you to use a small bag to carry your drain in, the ward can provide you with a small cotton bag.
How does the drain work?
A vacuum drain uses gentle suction. When the suction in the bottle is active, the green vacuum indicator on the top is in a downward (pressed) position.
The colour and volume of the fluid can be observed through the bottle, and this is of importance to your surgeon. As the area heals, the amount of fluid collected decreases until it is low enough for the drain to be removed.
Measuring the drain?
During your hospital stay, the amount of fluid collected in your drain is measured and documented in your notes at the same time every day. The fluid level is measured everyday by drawing a line and dating it.
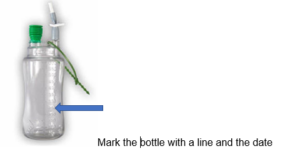
Your Nurse or Surgeon will show you how to care for your drain and also how to record the measurements on the chart within this leaflet so that you can monitor the output at home. To make this easier for you, the bottle has a measuring scale printed on it. Once you are at home, you will need to measure the fluid level each morning at a time that is convenient for you. We recommend measuring the drain at 8am. It is important that the fluid level is measured at the same time every day.
Possible problems?
If the following problems occur, please do not panic. Just follow the advice below:
- If the drainage bottle becomes too full or too heavy, you will need to contact the Breast Clinic to arrange for the bottle to be changed (out of hours Ward 16).
- The drainage bottle may lose its suction. Please do not panic as your drain will still work. However, it will need to be changed, you will need to contact the Breast Clinic to arrange for the bottle to be changed (out of hours Ward 16).
- The drainage bottle tubing may become detached. Place an absorbent pad (such as gauze) over the tube and secure it or reattach the tubing if you are able to. Contact the Breast Clinic immediately for further advice as the bottle will need to be changed (out of hours Ward 16).
- Excess leakage from the drain site, cover it with an absorbent pad and contact the Breast Clinic for further advice.
- Swelling or Redness to the drain site. Contact the Breast Clinic for further advice (out of hours Ward 16)
Removal of the drain?
The drain is normally removed when the fluid collected is equal or less then 50mls in a 24 hour period or at a date specified by your surgeon. You may need to contact the Breast Clinic to arrange this appointment or you may receive it prior to discharge from the ward
Tips
- Loose clothing that opens easily is generally easier to wear while you have your drain in.
- Ensure there are no kinks or folds in the tubing and the drain bottle is kept below the level of your heart.
- If applicable, a well-fitted, comfortable non-wired bra is helpful to reduce swelling and gives support after breast surgery.
- A small, comfortable pillow tucked under your arm (while you sleep or travel) may help to take pressure off the drain tubes and operation site.
- When lying in bed or sitting in a chair place the bottle upright on the floor
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Breast Clinic (01482) 622679. Monday – Thursday 8am – 4.30pm and Friday 8am – 12pm.
Alternatively you can email: hyp-tr.breastcareunit@nhs.net.
Outside of the clinic hours (evenings and weekends) please contact ward 16 (01482) 468616.
Drain Instructions
Drain can be removed in ______ days or when output is less than ______ mls / day.
Fluid Collection Record Chart
Please use the chart below to record your daily drainage output.
Drain:
| Day | Date | Daily Amount | Day | Date | Daily Amount |
| 1 | 8 | ||||
| 2 | 9 | ||||
| 3 | 10 | ||||
| 4 | 11 | ||||
| 5 | 12 | ||||
| 6 | 13 | ||||
| 7 | 14 |
Please use the chart below to record your daily drainage output should you have a second drain.
Drain:
| Day | Date | Daily Amount | Day | Date | Daily Amount |
| 1 | 8 | ||||
| 2 | 9 | ||||
| 3 | 10 | ||||
| 4 | 11 | ||||
| 5 | 12 | ||||
| 6 | 13 | ||||
| 7 | 14 |
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

