- Reference Number: HEY145/2023
- Departments: Breast Services
- Last Updated: 31 January 2023
Introduction
This leaflet has been produced to give you general information about your treatment following breast surgery with axillary involvement. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
Why do I need to do the exercises?
The exercises described in this leaflet are for anyone who has had breast reconstruction surgery. They have been approved by Breast Surgeons, Breast Care Nurses and chartered Physiotherapists. The exercises are designed for use in the days and weeks after your surgery, however it may be useful to practice them before your surgery so you know how to do them and what your range of movement is.
The exercises in this leaflet will help you regain the range of movement you had in your arm before your operation. Exercise may relieve pain as well as help the tissues heal, as during exercise more oxygen is delivered to the area being moved.
Can there be any complications or risks?
There is a small risk of muscle strain if you do not correctly follow the advice in this leaflet. It is normal to feel some muscle discomfort after exercising but this should improve after a couple of days. If it lasts any longer, then you should stop the exercises and consult your GP or Breast Care Nurse for advice.
Things to avoid after surgery
It is really important that you do not raise your arm above shoulder height for the first seven days following surgery.
Driving
Avoid driving until you have had your consultant review after discharge from hospital. However, if you need to drive, you must inform your insurance company.
Before driving, ensure you can turn the steering wheel fully, change gear, pull the handbrake on/off and perform an emergency stop.
Daily Activities
Avoid daily activities which involve heavy lifting, pushing, pulling or carrying – for example carrying bags of groceries, hanging out the washing or using the vacuum cleaner. You can gradually reintroduce these activities when you feel more comfortable, and for short periods, to begin with.
Avoid over exertion, do not strain and do not be over vigorous.
Avoid keeping the arm in one position for a long time.
How do I prepare for the exercises?
Please read the information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following your surgery.
When should I start the exercises?
The exercises should be started as soon as possible after your operation – the first day if possible. If you are not sure when to start, check with your surgeon or the physiotherapist.
Each exercise should be done three times a day. They can be done all in one session or broken into shorter sessions depending on your ability. You may find the exercises uncomfortable at first. Keep trying but do not overdo it.
If the exercise involves using only one arm, use the affected arm, that is, the arm on the same side as your operation.
How long should I do the exercises for?
You should continue these exercises until you feel you have gained your full range of movement, i.e. the range of movement that you had before your surgery. This should take about four to six weeks.
If you begin to develop stiffness in your arm after you have stopped these exercises, re-introduce them until this has eased.
If you have any concerns or questions regarding your surgery, please contact the Breast Care Nurse Team on tel: 01482 622013.
Exercises for day 1 to day 7
The following exercises should be carried out in a slow, rhythmical and gentle way to reduce the risk of lymphoedema (localised fluid retention and tissue swelling caused by compromised lymphatic system). If swelling does occur, contact your Breast Care Nurse.
 |
Sit with your arms down by your sides. Gently move your shoulder blades forwards and backwards, keeping your arms down by your side.
Repeat 5 times. |
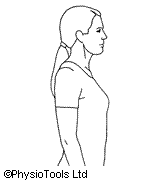
 |
Stand leaning on a table with your ‘sound’ arm. Let your operated arm hang relaxed straight down. Swing your arm forwards and backwards.
Repeat 5 times. |
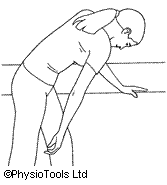
 |
Stand leaning on a table with your ‘sound’ arm. Let your operated arm hang relaxed straight down. Swing your arm across your body to your left and then to your right.
Repeat 5 times. |
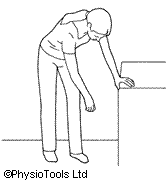
 |
Stand leaning on a table with your ‘sound’ arm. Let your operated arm hang relaxed straight down. Swing your arm as if drawing a circle on the floor. Change direction.
Repeat 5 times. |

 |
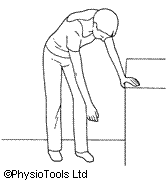
Stand or sit with the elbow of the arm, on the side which your surgery was performed, supported by your unaffected arm. Lift your elbow upwards towards the ceiling, assisting the movement with your other hand.
Do not let your elbow go above your shoulder. Repeat 5 times. |
Exercises to start 8 days after your operation
 |
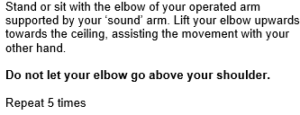
Sit or stand. Place your hand on your shoulder. Lift your elbow up towards the ceiling as far as possible.
Repeat 5 times. |
 |
Sit or stand with hands clasped in front of you. Lift both arms straight forward and up as far up as possible.
Repeat 5 times. |
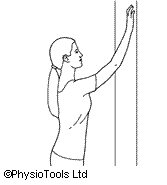 |
Sit or stand facing a wall. ‘Walk’ your fingers up the wall as high as possible. Reverse down in the same way.
Repeat 5 times. |
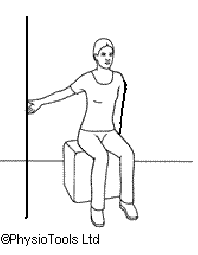 |
Sit or stand with the wall on your affected side. ‘Walk’ your fingers up the wall as high as possible. Reverse down in the same way.
Repeat 5 times. |
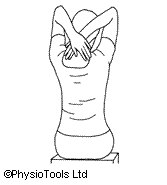 |
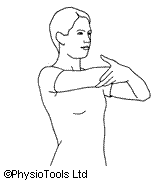
Sit or stand. Lift your hands up and cross them behind your neck, elbows pointing towards the ceiling. Move your hands towards your shoulder blades as far as you can.
Repeat 5 times. |
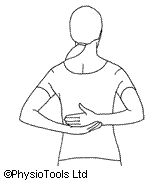 |
Sit or stand with arms behind your back, slide your operated arm up your back as far as possible. You can use your ‘sound’ arm to help if necessary.
Repeat 5 times. |
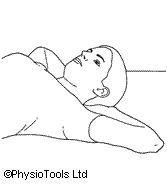 |
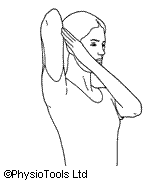
Sit in your chair or lie on your bed. Clasp your hands behind your neck with your elbows pointing outwards. Push your elbows back as far as possible to touch the back of the chair or the bed.
Repeat 5 times. |
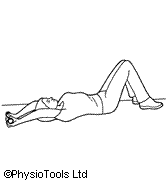 |
Lie on your back with knees bent. Link both hands and rest on your stomach. Lift your arms straight up and over your head to the bed, keeping your elbows as close to your ears as possible.
Hold approx. 20 seconds, remember to breathe normally and then return to starting position. Repeat 5 times. |
The above exercise is very important as this is the position you will need to adopt during treatment if radiation therapy is required following surgery.
Useful contacts
Breast Cancer Care
Kiln House
210 New Kings Road
London
SW6 4NZ
Telephone tel: 02073842984
www.breastcancercare.org.uk
Macmillan Cancer Support
89 Albert Embankment
London
SE1 7UQ
Freephone tel: 0808 808 2020
www.macmillan.org.uk
Breakthrough Breast Cancer
3rd Floor
246 High Holborn
London
WC1 7
Telephone tel: 08080 100 200
www.breakthrough.org.uk
This leaflet was produced by the Physiotherapy Department, Hull and East Yorkshire Hospitals NHS Trust and will be reviewed in January 2025.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.