- Reference Number: HEY963/2022
- Departments: Ophthalmology Department
- Last Updated: 30 April 2022
Introduction
This leaflet has been produced to provide you with general information about your treatment. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading this leaflet you have any concerns or require any further explanations, please discuss this with a member of the healthcare team who has been caring for you.
What is a dacryocystorhinostomy (DCR)?
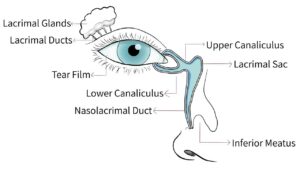
A DCR is a type of surgery that is used to treat blocked tear ducts in adults. It creates a new passageway between the tear duct sac and the nose, bypassing the blockage and allowing tears to drain normally again. The operation usually takes about one hour.
The operation is normally performed with the patient asleep (general anaesthetic) although, in very rare circumstances, this may not be appropriate and the eye may just be numbed (local anaesthetic). This will be discussed with you.
There are two types of procedure that can be used. The most suitable option for you will be discussed with you in the eye clinic when surgery is being offered and planned.
The two types of procedures are:
- External DCR – Is the most common operation for blocked tear ducts and has a success rate of over 90%. A small incision is made on the side of the nose to gain access to the tear sac. A small amount of bone between the tear sac and the nose is removed. A new passage is made for the tears to go down and some flexible tubes are placed in the new passage to keep it open. The tubes are usually removed after 6 – 8 weeks in the clinic. The stitches on the side of the nose will be removed after approximately one week.
- Endoscopic DCR – Uses a telescope to look up the nose and locate the site of the blockage, which is then opened up surgically. A flexible tube is inserted to keep the passage open, which again is removed after approximately 6 – 8 weeks. This method has the advantage of leaving no scar on the side of the nose, but the success rate is lower than with the external DCR (70%).
Your surgeon will discuss which operation is best for you.
Why do I need A DCR?
Normally, the tears that wash over the eye drain away through a system that runs from the corner of the eye to the inside of the nose. If there is a blockage in this system the eye can start watering and you may be more prone to infections.
To unblock the area, warm compresses and massage may be tried first. Sometimes it is also possible to unblock the tear duct by probing it. This is called syringing and involves flushing salty water down the tear duct. If the tear duct is open then you will taste the salty water in your throat.
What are the complications or risks of a DCR?
The main complications after surgery are bleeding and infection. It is also possible to displace the tube, which is inserted to keep the duct open and you may experience some bruising around the area of the operation.
A nosebleed may occur on the affected side. Usually this is a small amount and resolves within 48 hours. Excessive bleeding rarely occurs but if it does then a nasal pack may need to be used to stop the bleeding after the operation.
What happens before the operation?
In the outpatient clinic your tear draining passages will be assessed by syringing salty water through the tear ducts to find out where and how much of a blockage there is.
Once you and your surgeon have agreed that you should have a DCR operation then your name will be placed on the waiting list for the procedure.
How do I prepare for the operation?
Please read this information leaflet. Share the information it contains with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination.
Pre operative assessment
Before the surgery you will need to attend for a pre-operative assessment. At this visit you will be asked questions about your general health, some blood tests will be taken and a recording heartbeat (sometimes referred to as an Electrocardiogram – ECG) are performed to ensure your general health is good enough to undergo the surgery.
At this visit you will be given a suitable date for your operation.
Medication
We need to know what tablets and medicines you are currently taking also if you are hypersensitive to any substances. At the pre-operative assessment you will be advised on what pre-operative preparations you need to make such as altering medications.
If you are on warfarin or aspirin tablets it is important that you inform your surgeon, as these can lead to bleeding during or after the operation. You should stop your aspirin one week before surgery but the need to stop your warfarin will be discussed with you at pre-operative assessment.
Admission to hospital
You will generally be admitted to hospital on the day of your surgery, although in some circumstances you may need to be admitted the day before. This will be discussed with you.
What happens afterwards?
Immediately after the operation there may be a little discomfort, some spots of blood from the nose and some facial bruising at the site of the operation, (which would be expected to resolve within 2 – 4 weeks). Occasionally, a pressure bandage will be placed over the site of the operation to reduce the bruising. This will be removed before you go home. Usually you can go home the day after surgery.
After care
In order to prevent infection you will be prescribed eye drops or ointment for two weeks and possibly antibiotic tablets to take for 5 to 7 days. Some patients are also prescribed a nasal steroid spray twice a day.
The first clinic appointment is 7 to 10 days after surgery to remove the stitches if they have been used. The second appointment will be 6 to 8 weeks after surgery to remove the tubes in the outpatient department. A final check is usually made six months after surgery when you will be discharged if all is well.
If you do develop bleeding from the nose that will not stop, do not dab the nose but hold the end of the nose tightly. If bleeding carries on then attend your nearest casualty department immediately, also contact the Eye Clinic to let us know that you are having a problem on telephone number tel: 01482 816658 or tel: 01482 608788 (8.30 am to 5.00 pm, Monday to Friday) or Out-of-Hours tel: 01482 604346 (Please listen to full voice message on how to access emergency out of hours service).
Is there anything that I should avoid after the operation?
Important points to follow
Please remember the following points:
- During the first week after surgery you may get a little bleeding from your nose. In order to minimise this, you are advised to sit up rather than lie down and to sleep with extra pillows at night. You must not blow or pick your nose for one week after your operation. After that you are encouraged to blow your nose to clear the blood clots. If you need to sneeze, you are advised to do this with your mouth open.
- Avoid taking aspirin for at least ten days after surgery.
- For discomfort use pain relief medication that you would normally take for a headache.
- Also avoid exercise especially swimming for two weeks after surgery.
- Air travel is not advisable for at least seven days after surgery.
- Do not wear make up for two weeks after surgery.
- Avoid homeopathic medicines that promote fast healing.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Ophthalmic Department
on tel: 01482 816658 or tel: 01482 608788 (08:30 to 17:00, Monday to Friday)
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

