- Reference Number: HEY862/2024
- Departments: Gynaecology
- Last Updated: 30 April 2024
Introduction
This leaflet has been produced to give you general information about your treatment. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team caring for you.
How common are heavy periods?
It is a common condition; each year about one in five women aged between 35 and 49 years old consult their GP with heavy bleeding. Of all patients referred to a Gynaecologist, a third will have heavy periods. If present, the problem can disrupt women’s social, professional and intimate activities. It may lead to iron deficiency (anaemia) due to excessive blood loss.
What causes heavy periods?
A period occurs when the lining of the womb is shed every month. This lining, called the endometrium, always leaves behind a layer of cells from which a new lining will grow after each period. In roughly half of the cases there is no obvious explanation for periods becoming heavier. In other cases there may be an abnormality of the womb or there may be a hormone or blood clotting problem.
How do I know my periods are heavier than normal?
The symptom of heavy periods is difficult to assess. There is strong evidence which shows that half of the women who believe that their periods are heavy do in fact have normal periods. Your periods are likely to be heavy if you tend to use double protection with a sanitary pad and a tampon or change your sanitary protection frequently (between ½ and 2 hours), experience accidents with soiling your underwear, clothing, or soiling bed sheets.
What are the options for heavy periods?
Heavy periods can be treated medically or surgically. Commonly used medical options include combined contraceptive pills, tranexamic acid tablets, non-steroidal anti-inflammatory drugs such as mefenamic acid and the Mirena IUS.
Surgical options, which are usually performed if medical treatment fails to control the periods adequately, include endometrial ablation and hysterectomy.
In endometrial ablation, a variety of techniques are used to destroy the lining of the womb. Compared to hysterectomy, it is a much smaller procedure that is usually carried out as a ‘day case’. It will take you 1 to 2 weeks before returning to work.
Hysterectomy is the removal of the womb. It is a major operation requiring a general anaesthetic. A hysterectomy may require up to 5 days stay in the hospital and it may be 4 to 6 months before full recovery.
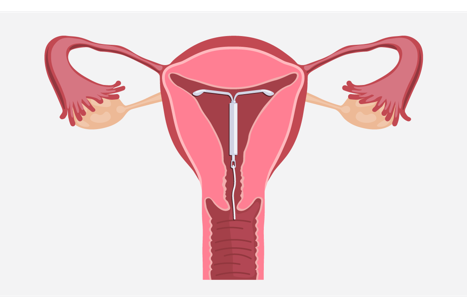
What is Mirena Intrauterine System (Mirena IUS)?
This is the most effective medical treatment for heavy and painful periods. It consists of a small, plastic T-shaped frame, which is inserted into the womb. This carries the hormone in a sleeve around its stem. The hormone is released gradually into the womb. The rate of release is controlled by a special covering on the hormone sleeve.
What are the advantages of having a Mirena?
The IUS is often used as a treatment for heavy periods, even in women who do not actually need contraception. It is also used as a treatment for endometriosis and fibroids. You do not require an operation or a general anaesthetic to have it inserted.
Once it is inserted you can forget about it and it can be used for contraception for 5 years. It does not interfere with sexual intercourse. Periods usually get lighter, less painful and often stop. After 12 months most users only have a light bleed for one day per month and about 1 in 5 users have no bleeding at all. Your own hormone levels remain the same and you will find that your periods return to normal after Mirena is removed. Not having periods or reduced blood loss can be an advantage to women’s health. Fertility returns as soon as it is removed.
Am I suitable for Mirena IUS?
Your Gynaecologist has to rule out other possible causes of heavy periods. Fibroids or polyps may be the cause of, or add to, your heavy bleeding. Some of these may require surgical treatment before you could be fitted with the Mirena. Mirena is a very reliable contraceptive and is therefore also suitable for women who need contraception.
How does a Mirena work?
The hormone in the Mirena IUS reduces the blood loss by thinning the lining of the womb.
How effective is it?
Mirena is an evidence-based treatment for heavy periods and is licensed for this purpose in the UK. There is strong scientific evidence that it greatly reduces the monthly blood loss in 9 out of 10 women users. The reduction of blood loss is gradual with more benefit as time goes on (86% reduction at 3 months and 97% reduction at 12 months after fitting). Many health specialists believe that the Mirena provides an important alternative to hysterectomy and other surgical treatments.
Would it affect the pain with my periods?
More than half of the women who suffer with heavy bleeding will have painful periods. Experience shows that Mirena will cure period pains in the majority (80%) of users, in addition to reducing the blood loss. About one fifth of women using Mirena will not have any periods at all. Some women find that because their periods are so much lighter after the initial few months, that panty liners provide adequate protection. If tampons are used, you should change them with extra care, so as not to pull the strings of Mirena.
How long does it last?
Mirena is a long-term treatment and can stay in for 5 years before it requires changing. Women who are in their forties will require one or two Mirenas before the menopause brings about a natural cure for their period problem. In many cases this means preventing the woman having to have a hysterectomy. If symptoms have not returned after 5 years of use, continued use may be considered. Your Mirena should be removed or replaced after a maximum of 8 years.
What about side effects?
The main side effect that occurs in all women is spotting (a small amount of blood loss) or light bleeding in addition to their periods for the first 3 to 6 months after the system is fitted. This may happen every day during the first 4 to 6 weeks after fitting.
Overall, you are likely to have a gradual reduction in the number of bleeding days and the amount of blood lost each month. For most of the time panty liners might be all that is required for protection, tampons may be used if needed.
The level of hormones in the woman’s blood stream is much lower than with the contraceptive pill, so the side effects such as tender breasts, headaches, acne, abdominal bloating or mood changes are less likely. If they occur, they tend to go away after a few months.
Will I put on weight?
Studies have shown that women using the Mirena IUS have not changed their weight any more than women not using it have.
Complications?
- Perforation of the womb at the time of fitting: very rare – 1 in 1000
- Low risk of either pelvic infection or ectopic pregnancies (pregnancy outside the womb)
- Risk of pregnancy (if you are using it as a contraceptive) is very low (under 1% – as effective as the implant). You need to contact your doctor if you think you are pregnant or if you have abnormal abdominal pain.
Can I change my mind?
You can ask the hospital team or your doctor to remove the system at any time. The removal is easy. If you are using the system as a contraceptive, it is important to use another reliable method of contraception in the week leading up to the removal and after the removal. Sexual intercourse during this week could lead to pregnancy after the system is removed.
Can it get dislodged or fall out?
This could happen in 6% (6 out of each 100) of all women who use the IUS. If this happens, you will lose your protection against pregnancy if you are using it as a contraceptive. Our experience showed that the majority of women who lost the IUS in this way might not feel or see it coming out and the only indication that this might have happened would be the sudden return of your heavy periods.
Please contact your doctor, or if necessary your Consultant Gynaecologist at the hospital, if this happens to you.
How can I check to see if it is in place?
After each period or about once a month, you can feel for the two fine threads of the system. It will be explained to you how to do this at the time of fitting. If you cannot feel the threads, contact your doctor or the hospital and in the meantime, use another reliable form of contraception. You may need an ultrasound scan to confirm the position of the IUS inside your womb.
You should also contact your doctor or the hospital if you can feel the lower end of the system itself or you or your partner feels discomfort during sexual intercourse.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the following departments based at the Women and Children’s Hospital:
- Gynaecology Outpatients on tel: 01482 607829
- Ward 30 on tel: 01482 604387
NHS Choices http://www.nhs.uk/conditions/Periods-heavy

