- Reference Number: HEY1536/2025
- Departments: Renal Service
- Last Updated: 31 March 2025
Patient Information Leaflet
Welcome to your Peritoneal Dialysis information booklet. Together with your Peritoneal Dialysis Community Nurse you will be able to work through the different sections to familiarise yourself with all aspects of your care so that you are able to safely carry out your dialysis at home.
Contents
- What is Peritoneal Dialysis (PD) and how does it work?
- Peritoneal Dialysis team
- Infection control
- PD start up regime
- Performing a manual peritoneal dialysis exchange
- Regular health checks in your own home
- Stores and how to order them
- Diet and fluid restrictions
- Problem solving
- Automated peritoneal dialysis machine (the overnight machine)
- Anaemia
- Useful Telephone numbers
What is PD and how does it work?
Normal kidney function
The kidneys filter the blood to remove excess water and waste. They also control blood pressure and the acid/alkaline balance in the blood. They produce the hormone erythropoeitin, which helps to make red blood cells, preventing anaemia (low blood count) and they help balance the calcium and phosphate in the blood to prevent the bones from becoming weak and protect blood vessels.
Peritoneal Dialysis (PD)
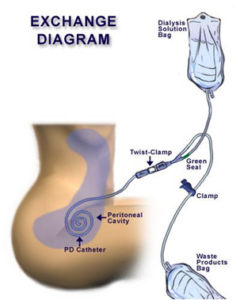
PD has been an established treatment for renal failure since the late 1970s. It is a treatment for patients with end stage kidney disease (ESKD). It is a method whereby the membrane, which lines the abdominal cavity, and its organs called the peritoneum (peritoneal membrane), is used as a filter to help remove certain toxins and excess fluid from the body.
It works by introducing fluid into the abdominal cavity via a tube permanently inserted into the abdomen, which is then drained in and out several times during the day (continuous ambulatory peritoneal dialysis (CAPD)) or during the night via a dialysis machine (automated peritoneal dialysis (APD)).
Most patients begin by having two manual peritoneal dialysis exchanges per day; one drained in at teatime and drained out at bedtime before another overnight bag of PD fluid is drained into the abdomen and left in overnight. This is usually increased as and when the patient needs more dialysis on an individual basis, to four bags daily.
Reproduced by permission from Baxter’s
The Peritoneal Dialysis Team
There are many people who are part of the renal healthcare team who may be involved with your care.
- Renal Consultants responsible for PD service
- Consultants, Specialty trainees, and junior doctors on the ward and in the regular clinics
- Peritoneal dialysis specialist community nurses (PD nurse) – will visit you in your home every 4 to 6 weeks, more often at first should you need them to.
- Renal Dietitians
- Renal Counsellor
- Renal Social Worker
- Ward 50 (in patient ward) staff
- Vantive support team – who supply your equipment and information
- Transplant team
Infection Control
Hand Washing Technique

Exit Site Care
Your exit site should be cleaned on alternate days.
- Gather equipment:
Topical exit site preparation as prescribed (write date and patient name on box when started, use only for that patient and at the end of each month discard).
- Hibiscrub or trust recommended solution
- Mupirocin cream as prescribed (write date & patient name on box when started)
- Saline sachet (Normasol)
- Sterile gauze squares
- Primapore/Mepore dressing(s)
- Mepore tape
- Alcowipe
- Wash hands as per hand hygiene protocol
- Clean dressing surfaces with Alcowipe.
- Open gauze & place on surface
- Place the gauze & Primapore packets on the dressing surface, peel off the top of the packets leaving the dressing material on the sterile remainder of the packet.
- Without touching the exit site, remove old exit site dressing & dispose of it correctly.
- Inspect exit site for any signs of infection or over granulation and take a swab for microscopy, culture & sensitivity if necessary.
- Wash hands.
- Take 1 piece of gauze, pour on the Hibiscrub and wipe around exit, down the catheter and away from the site.
- Take a 2nd piece of gauze and pour on saline, wipe around exit site, down the catheter and away from the site.
- Take a 3rd piece of gauze and dry the exit site in the same way.
- Put a pea sized amount of Mupirocin cream on the 4th piece of gauze and apply to the exit site.
- Cover the exit site with a dressing. Exit sites must be kept covered with a Mepore dressing until healing is complete, after this a patient may chose not to wear one as long as the exit has no signs of infection or discharge.
- It is essential that the catheter is anchored at all times with the tape supplied approximately 2 to 3 centimetres from the exit site dressing in the natural direction the line takes, ensuring the catheter is not under tension, bent or kinked (this applies even if no dressing is worn).
Routine peritoneal catheter exits site care undertaken if you are showering (Bathing MUST be avoided)
- Remove dressing before showering but ensure that the peritoneal dialysis catheter remains anchored with tape.
- Have a packet of sterile gauze and a bottle of Hibiscrub within easy reach of the shower.
- Shower as normal
- Wash hands
- Before turning off the shower open the gauze and apply 5 to 10mls of Hibiscrub. Clean around the exit site then down the peritoneal dialysis catheter away from the body.
- Rinse the soap off with the shower.
- Once out of the shower dry as normal avoiding the exit site area.
- Lastly dry the exit site with a piece of sterile gauze.
- Cover the exit site area with a Mepore dressing if required.
- Renew the anchor tape with Micropore tape.
Exit Site Infection
Should you suspect that you have an exit site infection, please contact the PD office or your PD nurse.
Symptoms
- Redness
- Discharge from the exit site
- Soreness
Infected exit site Healthy exit site


There is evidence to suggest that Mupirocin/Fucidin/Naseptin cream applied to the exit site each time it is cleaned helps to reduces episodes of peritonitis. It has also been found that Mupirocin ointment applied to the nostrils twice per day for the first 5 days of every month can also prevent peritonitis. If a scab forms on the exit site, do not remove it; allow it to heal and come away on its own
DAILY ACCESS CHECK FOR PD
- LOOK AT AND FEEL your stomach /abdomen for unusual:
Swelling Redness/warmth Discomfort Wetness Discharge Bleeding
- CLEAN daily and additionally after swimming, showering, becoming wet or dirty
- SECURE by anchoring to avoid pulling, trauma and irritation at exit site
- INSPECT drain bags, they should look clear – see problem solving if cloudy or you are unsure.
PD start up regime
When patients first start peritoneal dialysis (PD), usually they have enough residual renal function (work that the kidney is still doing) to allow for a reduced PD regime. We call this the start-up regime.
This regime consists of a PD exchange at between 6 to 7pm, with a 3 to 4 hour dwell period; followed by an overnight PD exchange. This stays in (dwells) in all night and is drained out in the morning. The patient is then left dry (without any dialysis fluid in) during the day. Dialysis recommences at 6-7pm the following day when dialysis fluid is once again instilled into the peritoneal cavity.
By not giving you more dialysis than you need, we are attempting to extend the time that you can use peritoneal dialysis (PD) as your treatment choice. Unfortunately, some patients that have a very low residual renal function (may not pass much urine) when commencing PD, are not suitable for the start-up regime and will need to start on the full PD regime (usually 4 exchanges day). The start-up regime is just that, a start-up regime. As time goes on your renal function may decrease and your dialysis will need to be increased to meet your changing clinical needs. Patients stay on the start-up regime for different lengths of time because residual function will decrease at different rates for different individuals. The average length of time spent on the start-up regime is six months, with a few requiring increased dialysis after one month and a few staying on the regime for over two years.
Your Dialysis Nurse will use the results of the blood tests and adequacy testing to determine if the start-up regime is enough dialysis, to meet your needs or whether you may need to increase the amount of peritoneal dialysis you do.
Performing a manual peritoneal dialysis exchange
It is very important to keep the area where you perform your dialysis clean and dust free and to keep all the room doors and windows closed. Please do not allow people to open the door and keep pets out of the room.
Please carefully check the individual packaging of each peritoneal dialysis fluid bag, (cap and shield etc.) before opening to ensure that it is intact, in date and that the fluid is clear. If anything is damaged, dispose of it in the yellow clinical waste bags.
Warm your dialysis bags on the warming plate supplied or on the top of your APD machine and not on a radiator in a microwave or in hot water as this may cause it to have hot spots and can damage the fluid. Do not remove the outer wrapper from your dialysis fluid bag whilst warming.
Step 1: Connect bag
- Close all windows
- Gather equipment – bag of warmed dialysis fluid (check date, volume and strength), clam shell, blue grippers, alcohol wipes, alcohol gel and cap
- Get your peritoneal catheter out from your clothes
- Wash your hands thoroughly
- Wipe your surface using an alcohol wipe and ever increasing circle technique
- Open the bag package and put it on the surface with the lines upper most
- Open the clam shell packet
- Apply alcohol gel to your hands
- Pull lines out straight and peel off drain bag
- Pull the coloured tag off the end of the lines
- Carefully fasten the clam shell on the end of the line. Do not touch the exposed end of the bag with your hands or clothing
- Pick up your peritoneal dialysis catheter and remove cap, placing it on the open clam shell pack. IT IS IMPORTANT THAT NOTHING (EG CLOTHING) TOUCHES THE NAVY BLUE END OF YOUR CATHETER
- Carefully screw the fluid bag line to the end of your catheter, holding both ends from the top so that your fingers cannot touch the ends. Keep tight hold of your PD catheter and twist the bag onto it
Step 2: Drain
- Hang the fluid bag up
- Place drain bag on the floor
- Open your patient valve and allow the fluid to drain out
N.B. If this is your first bag of the day you will not expect any fluid to drain out, but you should always perform the drain out stage to avoid accidental overfill
Step 3: The Flush
- Close the patient valve
- Have blue gripper ready to put on the drain line
- Break the green seal and allow fluid to drain into the drain bag for 10 seconds
- Put blue gripper onto the drain line
Step 4: Drain in
- Open your patient valve and allow the fluid to drain from the fluid bag to your abdomen
Step 5: Cap off
- Close your patient valve
- Put the second blue gripper on the fluid line
- Wash hands thoroughly
- Wipe the surface with an alcohol wipe using ever increasing circle technique
- Open the cap packet
- Apply alcohol gel to hands
- Pick up your peritoneal dialysis catheter in one hand and the fluid bag line in the other and disconnect them from each other
- Keep hold of your peritoneal dialysis catheter and drop the fluid line onto the floor
- Pick up the cap with the empty hand and screw it onto your peritoneal dialysis catheter without touching the sterile end.
Drain out only
- Close all windows and doors
- Gather equipment: Empty drain bag, clam shell, cap, alcohol wipes and alcohol gel.
- Get your peritoneal dialysis catheter out from your clothes
- Wash your hands thoroughly
- Wipe the surface using alcohol wipe and ever-increasing circle technique
- Open your drain bag, leaving it on the package on your surface
- Open the clam shell
- Apply alcohol gel to your hands
- Pull the light blue cap off the end of the drain bag, put the clam shell/shield onto drain bag and replace it onto the sterile packet
- Pick up your peritoneal dialysis catheter and remove cap
- Connect the drain bag to your peritoneal dialysis catheter with the same care used whilst connecting PD fluid bags
- Remove paper tab, allowing drain bag to sit on the floor/stand
- Undo patient valve and allow fluid to drain out
- When you have completely drained out clamp the drain bag line using the white clamp that is already on the line and your patient valve
- Cap off as per the instructions given in Step 5, steps 3 to 9
Regular Health Checks in your own Home
You will be assigned your own Specialist Community Peritoneal Dialysis Nurse who will usually visit you at least once a month. He/she will usually carry out the following tests:
- Blood Pressure
- Weight
- Check of your exit site
- Check of your ankles/legs for oedema (swelling) and ask you if you have any symptoms of shortage of breath
- Give advice about your dialysis regime
- Ask about the colour of your peritoneal dialysis fluid
- Ask about your bowels
- Answer any queries you may have
- Carry out blood tests. These may include:
- Full Blood Count (FBC) – checks your red and white blood cell count and your haemoglobin (Hb). This is a check for anaemia (low blood count).
- Biochemical Profile (BCP) – checks the levels of toxins in the blood (e.g. potassium, phosphate, creatinine, urea and calcium).
- And less regularly:
- Cytotoxics – if you are on the transplant list.
- Parathyroid Hormone – see section on diet and fluid restrictions.
- Glucose – usually only as part of the Peritoneal Equilibrium Test (PET) and adequacy tests (see later). If you are a diabetic your diabetic nurse may check your blood glucose more regularly.
- Ferritin and transferrin saturation (TSAT’s) – these tell us if we need to give you iron.
- Hepatitis and HIV – for infection control purposes.
Patients are now able to view their own blood results on their home computers via Patient Know’s Best (PKB). The low clearance nurses may have already got you started with this but please ask your dialysis nurse for further information. Your dialysis nurse will inform you of your monthly blood results and discuss these with you.
Adequacy Test
After about 4 weeks on PD and then again, every three to six months, your nurse will need to carry out an adequacy test. You will be asked to save all your urine for 24 hours prior to your arrival. On the day before the test, we ask you to pass the first urine of the day in the toilet in the usual way, then to save all of the rest of the urine you pass, up to and including the first urine passed on the day of the test, in a clean container.
Also, your nurse will ask you to save all your dialysis fluid from the last 24 hours. This could be as simple as not stripping down your dialysis machine until the nurse gets there, or saving one, two or three manual bags from the previous day and the drainage from the overnight bag on the day of the test.
The results of this test can determine your fluid allowance (see section 7) and will let us know how much work your kidneys are doing and how much work your dialysis is doing. From this, we will know if your dialysis needs increasing (or very occasionally decreasing).
Your nurse may also perform this test after an episode of peritonitis or if your blood figures change suddenly.
Peritoneal Equilibrium Test (PET Test)
After about 4 weeks on PD and then on further occasions depending on how your PD is going, your Dialysis Nurse will perform a PET test and a set change, in your own home. The set change is simply a change of the end piece of your peritoneal dialysis catheter under extremely sterile conditions. You do not need an operation for this.
The PET test tells us whether your peritoneum dialyses quickly or slowly and allows us to work out the best dialysis regime for you. The nurse will be at your house for approximately five hours to complete the test. He/she will take blood samples from you as part of the test.
The PET test will require you to use a 2.27% strength (green) dialysis exchange the night before the PET test. This should be put in at least 10 hours before your nurse arrives.
You will need to have another 2.27% (green) bag warmed and ready to use when your nurse arrives on the morning of the test. Please do not do your dialysis or drain out until your nurse gets to your home.
Continuous Training
Every three to six months (or following treatment for any infections) your nurse will go through your hand washing technique with you and check that you are still following the aseptic dialysis technique correctly. It is easy to forget the precise method for connecting yourself to the APD machine or manual exchange over time and it is very important that it is done correctly to prevent peritonitis.
Stores and How to Order them
- The healthcare suppliers, Baxters, supply your dialysis fluid and other necessary equipment.
- You will be sent a list of the dates when a Vantive representative will phone you for your order and when they will make your delivery. They will ask you what stores you have remaining and will work out what you need.
- You will receive your delivery a week later. The driver who delivers it will carry your dialysis fluid and equipment to wherever you want it storing in your home, shed or garage, as well as rotating your stock.
- Most people are at home for their delivery but, if you are out, a key to an outhouse/shed can be left in a place known only to yourself, Baxters and the delivery driver.
- There is a text messaging service to remind you of your delivery date.
- It is very important to order enough dialysis fluid each time, including any ‘just in case’ fluid as it is extremely difficult and very expensive, to get any fluid delivered later as an emergency.
- You will be issued with a sharps bin by Vantive, which your Dialysis Nurse may occasionally use to dispose of needles. Please keep this out of the reach of children. It can be disposed of by your Dialysis Nurse and should not be put out with the household waste.
- The fluid from your used dialysis fluid bags should be emptied down the toilet and the empty bag and all other dialysis related rubbish put in the yellow clinical waste bags. Your Dialysis Nurse will arrange for your council to collect it from your home on a set day every week.
Holidays
Being on peritoneal dialysis does not mean that you are unable to go away on holiday as Vantive can deliver to most countries and to anywhere in Great Britain. We just ask that we have at least 6 weeks’ notice to plan for fluid delivery to your destination. There may be a charge if the notice period is less than this. It is always wise to take one manual bag and a few shields, caps and other useful bits and pieces with you in case of hold ups on your journey. Vantive holiday club phone number is at the end of this booklet. It is important to check with the PD team before you book any holiday that we are happy you are fit to travel.
Diets and Fluid Restrictions
Target weights
When you have become settled on peritoneal dialysis your nurse will set you a target weight. This is the weight that we think you should be when you have no excess fluid in your body, and you are not dehydrated (too dry).
Fluid overload
Your kidneys may no longer be able to get rid of enough fluid from your body. If this happens you will be asked to drink less fluid. This is known as a fluid restriction/ allowance. If less fluid is taken into your body by mouth, then there is less that must be removed by dialysis, particularly if you no longer pass much urine. Your PD nurse or dietician will advise you how much you are allowed to drink each day and give you some tips on how to cope with your fluid restriction. For example, taking a low salt diet, sucking ice cubes etc.
Generally, your fluid allowance should be roughly the amount of your previous day’s urine output plus an extra 500ml.
You may also be instructed to use stronger dialysis fluid – 2.27% (bags with green tags) or even 3.86% (bags with orange tags), although overuse of strong fluid may gradually shorten the time that peritoneal dialysis will be effective for you.
Symptoms of fluid overload:
- Breathlessness
- Swollen ankles, puffy face or other body parts
- High blood pressure
- Rapid increase in weight

This does not mean that you cannot increase/decrease your body weight. A more gradual weight change would indicate a change in body mass (i.e. muscle or fat) and not fluid and your PD nurse could alter your target weight accordingly. Your blood pressure, along with any oedema (swelling, for example on your ankles), will also help your PD nurse to decide if your weight change is due to excess fluid in your system.
It is very important to keep your blood pressure within normal limits as high blood pressure (hypertension) can cause heart problems and/or strokes (cardiovascular disease).
Dehydration
Occasionally people with chronic kidney disease become dehydrated. In this case you may be asked to drink more fluid and to use 1.36% (bags with yellow tags) or Nutrineal (bags with blue tags).
Symptoms of dehydration:
- Low blood pressure
- Reduced weight
- Dry mouth and skin
- Dizziness – although this can be caused by other conditions such as anaemia (low blood count)
Diet
As your kidneys can no longer get rid of many of the electrolytes (toxins) in your blood, you may be advised to go on a special renal diet. This may be a low potassium or a low phosphate diet, or both. The dietitian will tell you which type of diet you have to follow to remain healthy and will offer dietary advice over the phone or in the clinics.
Potassium – this is found in bananas, tomatoes, coffee, mushrooms and other foods indicated on your diet sheet. These foods are not restricted in every patient. If potassium is found in large amounts in your blood stream it can cause arrhythmias (irregular heartbeat) and your nurse may ask you to come into hospital to correct your potassium levels.
Phosphate – this is found in dairy produce, i.e. milk, cheese, nuts and other foods indicated on your diet sheet. If it is found in larger than normal amounts in your blood stream it can cause itching and, if it is not controlled, over time it could leach calcium from your bones and cause them to crumble. The calcium can collect in your blood vessels, calcify (harden) and constrict them, causing cardiovascular problems. You may be prescribed phosphate binders (tablets) to help to control your phosphate and these should be taken at the same time as your meals, as they stop the phosphate in your gut from entering your blood stream.
Calcium – this can also affect your bones and cause calcium build up. It may be an indication that your parathyroid glands (situated near your thyroid gland) may not be secreting the correct amount of parathyroid hormone. Your consultant will discuss with you the treatment plan, which may be surgery.
Problem solving
Peritonitis – this is an infection in the peritoneal cavity. It is potentially very serious but if you act immediately, it can often be treated before you become unwell. At the first sign of any of the symptoms below contact the Peritoneal Dialysis Team in their office or via Ward 50. The PD staff will take blood and PD fluid samples and administer antibiotics. Delay in seeking help from the PD team may result in a stay in hospital, damage to your peritoneum or, in the worst case, removal of your PD catheter, resulting in a time on haemodialysis, hopefully on a temporary basis.
Symptoms of peritonitis
- Cloudy or hazy peritoneal dialysis fluid
- Abdominal pain
- Nausea and/or vomiting
- Diarrhoea
- Shivering and high temperature

Drainage problems – If your peritoneal dialysis fluid does not all drain out or drains in or out very slowly, or if your APD machine alarms and shows “low drain” then you are having drainage problems. There are several reasons for this:
- Constipation – solved by taking extra laxatives. This is the most common reason for drainage problems. You should already be taking some laxatives regularly as prescribed but may need something stronger; your PD nurse will advise you. You may still be constipated even if you are opening your bowels regularly but not adequately. Strangely, diarrhoea can be a symptom of constipation, as it could be due to unformed stool bypassing the blockage. Very severe constipation can cause peritonitis and/or PD catheter displacement, so should be treated as soon as you notice a problem. Sometimes an abdominal X-ray may be done to investigate this. The Bristol stool chart (a picture chart) can give you some idea of what your stool (poo) should look like, and your PD nurse may discuss this with you
- Displaced PD catheter – if you have been very constipated for some time your catheter may move to the top of your abdomen and cause drainage problems. If it is still out of place once the constipation is resolved it can only be rectified by surgery.
- Fibrin – this is a substance made by the body to help stop a small bleed. The bleed may have been caused by heavy lifting or coughing. It is a white or sometimes blood-stained substance found in drained PD fluid and is nothing to worry about unless it blocks your PD catheter and causes drainage problems. Your PD nurse will add a drug called Heparin to your PD bags to disperse the fibrin and prevent further problems.
Blood-stained fluid
If your drained out PD fluid is blood stained or pinkish in colour, please do not panic. it does not take much blood to make the fluid look very red. If you are female this may be related to your period.
It may be that you have previously lifted something or carried out some physical activity that has caused a tiny bleed within one of the small blood vessels in your peritoneal cavity. This usually heals without anything needing to be done. Contact the PD office immediately and they will advise you what, if anything, you need to do.
Exit Site Infection – See Section 3 (Exit Site Care)
Hernias and Leaks – Sometimes the pressure of PD fluid in the abdomen can find a weak area in the abdominal wall and cause a hernia. Alternatively, the PD fluid can find a way to leak out into your scrotum, the tissues of your abdomen, up into your chest or out via the exit site. If you find a swelling, become breathless or find that your exit site is wet, please inform your nurse or phone the PD office. This is quite rare but worth mentioning if suspected.
Split Lines or Detached Set – this is rare. Sometimes the end piece of your PD catheter may become disconnected, or your line may become worn and split above the titanium connector. If this happens:
- Clamp the line above the split/disconnection with a blue clamp
- Do not drain any PD fluid in
- Cover the split/end with sterile gauze and tape
- Contact the PD staff immediately to arrange to attend the hospital for a new set or line repair
It is a good idea to check that the set is screwed on tightly every few weeks so that it does not become loose.
Automated Peritoneal Dialysis Machine (The Overnight Machine)
When you first start on peritoneal dialysis you will usually stay on the manual PD bags for a while to get you used to the technique and the feeling, after which you may need to move to APD (the overnight machine).
APD completes several exchanges whilst you sleep and leaves some long-acting dialysis fluid in during the day. Your PD nurse will want you to do a PET and adequacy test before you start on APD. Your PD nurse will work out the most suitable dialysis regime for you based on the tests that she/he performs.
Anaemia
The healthy kidney produces erythropoietin (EPO), a hormone, which stimulates the bone marrow to produce red blood cells. This is often reduced in patients with chronic kidney disease and means that these people are more likely to be anaemic. Anaemia means having low haemoglobin (Hb) and fewer red cells in the blood. These carry oxygen around the body. Blood tests may reveal a low folic acid, vitamin B12 and/or iron, all of which can also cause anaemia but can be increased with medication. Erythropoietin can be replaced or increased by injecting a similar substance often referred to as Aranesp or Erthytrocyte Stimulating agent (ESA) or sometime using medications taken by mouth.
Before starting EPO injections or oral medication, your doctor or PD nurse will check that you are not bleeding from anywhere (such as your bowels or having heavy periods) and will check for any infections such as a urinary tract or exit site infection, both of which can cause a drop in Hb. Severe anaemia can be treated by blood transfusion, although this can have implications for kidney transplantation in the future.
Symptoms of Anaemia
- Breathlessness
- Insomnia
- Tiredness/lethargy
- Irregular heart beats
- In severe cases – chest pain
Useful Telephone Numbers
Peritoneal Dialysis Office: – tel: 01482 674979
Ward 50: – tel: 01482 675050
Vantive order number: – tel: 0800 0234 002
Vantive APD Machine Support Team: – tel: 01635 201902
Vantive holiday club – tel: 0800 0234 002 option 3
Please inform the PD Department if you are admitted to hospital for any reason, even if it is unrelated to dialysis or renal problems. This will enable us to arrange your dialysis promptly. It may also be wise to make sure that the staff on the ward you are admitted know that you must regularly take laxatives and are on anaemia medications and need to take your phosphate binders with your meals, if you have been prescribed them.

