- Reference Number: HEY663/2025
- Departments: Neurology and Neurosurgery
- Last Updated: 31 January 2025
Introduction
This leaflet has been produced to give you general information about your condition. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team but may act as a starting point for discussion. If after reading this leaflet you still have concerns or require further explanation, then please discuss this with a member of the healthcare team.
What is the pituitary gland?
Structure: The pituitary gland is a pea-sized hormonal gland that sits in a small hollow in the base of the skull immediately under the brain and behind the eyes. It is not part of the brain but is connected to it by a ‘stalk’. The pituitary stalk contains special blood vessels through which the brain sends hormonal messages to control the function of the gland. Across the space between the pituitary gland and the brain lie the nerves connecting the back of the eyes to the brain (the ‘optic nerves’). A pituitary tumour can touch, press and stretch on the optic nerves. This can affect the signal from your eyes to your brain and may affect your eyesight.
Function: The pituitary gland controls a number of different hormones (chemicals) affecting different body systems. These include cortisol (a steroid hormone, which is responsible for a wide range of body functions); thyroid hormone (which controls your metabolic rate); sex hormones (for sex and reproduction); prolactin (for breast milk production in women); growth hormone (for growth during childhood and adolescence) and anti-diuretic hormone (for water balance).
What are pituitary tumours?
Pituitary tumours, also known as ‘adenomas’, are benign (non-cancerous) growths in the overwhelming majority of cases. Less than 1 in 100 of pituitary growths are cancerous. Other growths come from pituitary tissue, or rarely from the surrounding tissues. Pituitary growths do cause similar symptoms. A large pituitary tumour can compress on the optic nerves and affect the eyesight. It can also cause damage to the surrounding normal pituitary tissue and result in deficiency of some or all of the hormones produced by the pituitary gland.
Infrequently, an adenoma may produce hormones abnormally. The most common is a prolactin-producing tumour (also called ‘prolactinoma’). Other functioning adenomas produce steroid hormones (causing ‘Cushing’s disease’) or growth hormones (causing ‘acromegaly’).
What does pituitary surgery involve?
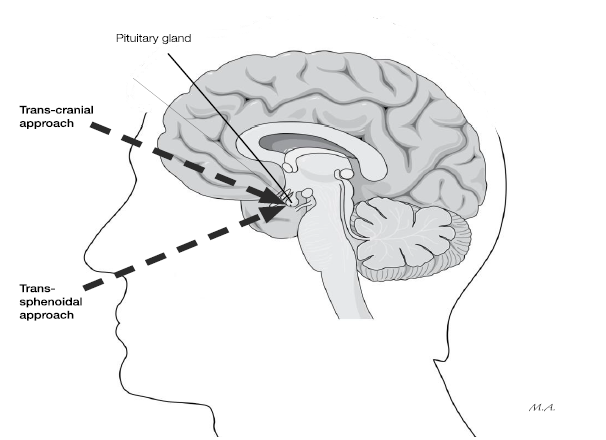
Most operations on the pituitary gland are carried out through the nose. This gives the surgeons easy access to the gland with minimal injury to the patient. It is called ‘trans-sphenoidal surgery’ as the pituitary gland sits within a protective bony hollow on the ‘sphenoid’ bone, at the back of the nose. This is the most common type of surgery for a pituitary adenoma. Occasionally, the surgeon may need to reach the tumour by exposing the brain through the skull. This is called ‘trans-cranial surgery’.
You will be given ample opportunity to discuss benefits and risks and ask related questions. You will also be given time to think things over and to discuss with family or friends. We will operate only after you have given consent.
The benefits of the surgery will be discussed with you before the operation. In most cases, surgery is a planned (elective) procedure. Common reasons for surgery are:
- To save your eyesight when a tumour is pressing on or stretching the optic nerve.
- To stop over-production of abnormal hormones in Cushing’s disease, acromegaly or very rarely, prolactinomas.
- To relieve pressure when the tumour bleeds into the pituitary gland (‘pituitary apoplexy’). This can lead to problems with vision, although this is a very rare occurrence. We would normally aim to do surgery urgently to prevent further deterioration.
What are the risks of surgery?
The risks of surgery will also be discussed with you before the operation. There are many steps that we take to try and stop complications happening and things that we do to reduce the impact of such complications when they do happen. When complications do occur, they are usually treatable.
Possible complications of surgery are:
- Nasal pain or blockage, decrease in sense of smell, crusting that needs nasal douching, septal perforation.
- Bleeding, infection including meningitis, leakage of the fluid that bathes the brain from the site of operation (CSF leak) and hormonal abnormalities such as water imbalance or low steroid production requiring lifelong hormone replacement.
- If we do get a CSF leak, we occasionally take a piece of fat and plug the hole and then put a drain in the spine to divert the fluid away temporarily, while the hole undergoes repair. This might require further treatment and could mean a longer hospital stay.
- There is also the risk of blindness, double vision and stroke.
- Any brain operation carries a very small risk of death as a complication, which is less than 1 in 1000.
What will happen?
Your operation will take place in the Neurosurgery Unit at Hull Royal Infirmary.
You will be admitted before the operation. You can eat and drink normally throughout the day prior to admission. You will need to fast before the operation. Staff on the ward will provide detailed instructions in this regard. The actual operation will take approximately two hours, but you will be away from the ward for a longer period than this, as you will go to the pre-surgery and recovery areas. You will be put to sleep under general anaesthesia during the operation. You will be monitored closely on the Neurosurgery High Observation Ward.
What happens afterwards?
In hospital:
- You will probably have nasal packing for a few days as an inpatient.
- You will have blood tests more or less daily after the operation.
- You can expect to be discharged within 3 to 5 days after the operation.
- You may also have your eyesight checked and a brain scan done.
The hormones that regulate water balance can be affected by the operation. This can lead to water imbalance, with too much urine, or too little urine being passed. Usually, the imbalance settles in a few days but you may need treatment to correct it and may need to stay in hospital for longer.
You will be discharged with a medicine called hydrocortisone. It is important that you take this medication as prescribed. Usually, this is 10 mg (1 tablet) in the morning at breakfast, 5 mg (½ tablet) at lunch and another 5 mg (½ tablet) in the evening, no later than 6pm. You must remain on hydrocortisone unless and until you are advised to stop by your endocrinologist or the endocrine clinical nurse specialist. If stopped inappropriately, it could be potentially life threatening.
You should avoid blowing of your nose or sneezing for three weeks after surgery.
At home:
You should be able to continue with normal daily activities but will need to do these more gently in the recovery time. It is usual to have 4 to 6 weeks recuperation and recovery from surgery. Recovery times do vary from person to person.
If you have had visual problems due to the tumour, then you must inform the DVLA and your insurance company that you have had surgery. This is a legal requirement and could invalidate your insurance if you do not. You may need an eye test before you can drive again after surgery. More information is available on the DVLA website (see below) and in most cases, you can continue to drive if vision has not been an issue.
1 to 2 weeks after surgery, you should attend your doctor’s surgery for blood tests on two separate days. The clinical nurse specialist will give you two blood request cards for tests.
You should book an appointment with your doctor surgery for the blood samples to be drawn. The time for the blood test should be at 9.00am ideally but acceptable between 8.00am and 10.00am. Natural steroid hormone levels are highest in the morning. Blood tests done late in the morning or in the afternoon are not helpful in making treatment decisions.
Once you have booked time for the blood test, it is important that you do not take the hydrocortisone medication no later than 6pm the night before, or on the morning of this test, unless your endocrinologist tells you otherwise.
You should take hydrocortisone tablets as normal after the blood tests are done.
Your endocrinologist or the clinical nurse specialist will let you know the result of the blood test. The result could take a few weeks. If the result shows that you have good steroid hormone levels, you will be advised to stop the hydrocortisone tablets. If you have clearly low levels, you will be advised to continue on the hydrocortisone tablets long term, probably for life. A large number of patients fall somewhere in between. In that case, further testing at the Medical Day Unit will be arranged. This may be at Hull Royal Infirmary or at your local hospital if you are not from Hull or the East Riding.
In approximately 6 weeks, you will be asked to come to the joint Neurosurgery Endocrinology clinic for a post-operative assessment.
3 months after surgery, you will have an MRI scan to assess the result of the surgery and whether adequate tumour has been removed. The MRI may be done in your local hospital if you are not from Hull or the East Riding. We will discuss the results of the MRI scan in our monthly specialist meeting and feedback the results to your GP, your Endocrinologist and you.
4 to 6 months after your surgery, you will have an appointment with your endocrinologist. This will be in Hull if you are from the local area or in your referring endocrine unit in your local hospital.
Future appointments may be made every 6 to 12 months depending on your clinical needs.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Neurosurgery Department as follows:
Consultant Neurosurgeons on tel: 01482 604477 or tel: 01482 604319
Clinical Nurse Specialist in Endocrinology on tel: 01482 675360
Clinical Nurse Specialists in NeuroOncology on tel: 01482 607831
Neurosurgical Ward on tel: 01482 675004 or tel: 01482 674777
The Pituitary Foundation
Patient Information and support helpline: tel: 0117 370 1320 (Monday to Friday 10am to 4pm)
Endocrine Nurse Helpline: tel: 0117 370 1317 or tel: 0845 450 0377 (Monday 8.30am to 1.30pm, Tuesday 11am to 4pm, Wednesday 6 to 9pm)
Helpline Text Service: tel: 07786 202 249 Monday to Friday, reply will come from ‘Pituitary’
E mail: helpline@pituitary.org.uk
Website: www.pituitary.org.uk
DVLA website: https://www.gov.uk/dvla-medical-enquiries

