- Reference Number: HEY1456/2024
- Departments: Gynaecology
- Last Updated: 31 October 2024
Introduction
If you are reading this leaflet because you have lost a pregnancy or baby, we are so sorry, and we will do all we can to provide you with the support that you need during this difficult time. The information within this leaflet is designed to help you to understand what may/may not happen following your pregnancy loss. We understand this is a distressing time for you and your family. Everyone’s experience is personal to them and will vary from one individual to another. The information below is to help guide you through the process and to reassure you that you can seek help and support at any stage should you wish to do so. Throughout this leaflet we will refer to the loss as a ‘pregnancy’. We are aware that this is also very personal and we do not intend to cause any unnecessary distress by doing so.
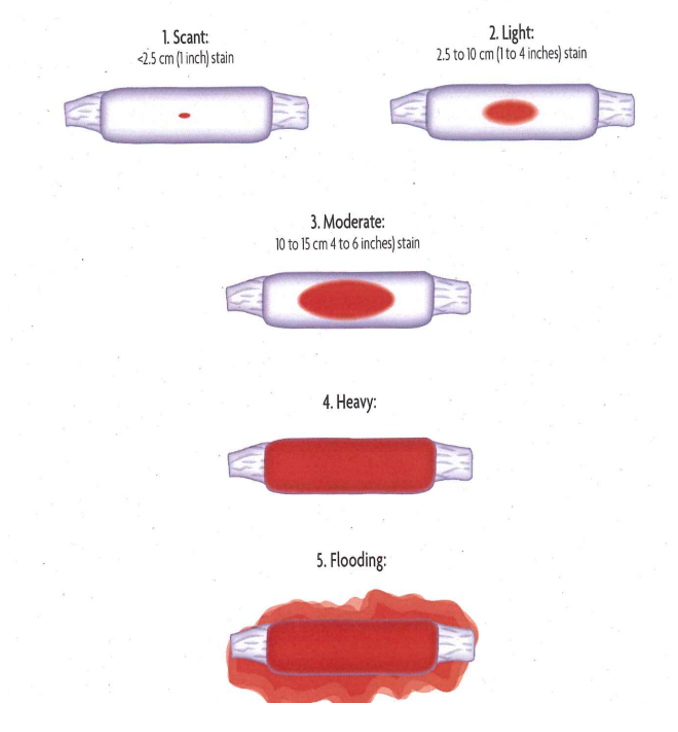
Most women experience some vaginal bleeding during a pregnancy loss. The amount of bleeding you have will usually depend on how many weeks pregnant you are. It may be very heavy at first and you may pass large blood clots and pregnancy tissue. It may last up to 4 weeks after you have passed your pregnancy, depending on how many weeks pregnant you were. The bleeding should get lighter and may become brown in colour.
We advise to use sanitary towels or period pants rather than tampons or menstrual cups. Putting anything inside your vagina when you are bleeding after a miscarriage can increase the risk of infection.
Contact the Early Pregnancy Unit on: tel: 01482 608767 (between 08.00 am and 17.30 pm Monday to Friday) and (between 08:00 am and 15.30 pm Saturday/Sunday/ Bank Holiday’s) OUT OF THE ABOVE HOURS CONTACT: tel: 01482 604387 if:
- the amount of bleeding makes you feel unwell, dizzy, faint or frightened;
- you are having to change a heavy flow sanitary pad more than every hour for more than a few hours;
- you have a fever (a temperature above 38˚C);
- you notice a foul smelling vaginal discharge.
Many women also experience cramping during a pregnancy loss. This is your body’s way of helping you to pass the pregnancy.
- Your womb will contract to help you to pass your pregnancy. Some people describe these as strong period pains. You can use over the counter pain relief medication such as (paracetamol or ibuprofen) to help reduce the pain. Heat packs can also be used.
- Most women can manage at home but some women may need to call 999 and attend hospital as an emergency as they cannot manage their pain relief and/or they may be experiencing very heavy vaginal bleeding. In the event of very heavy vaginal bleeding (referred to as 5. ‘Flooding’) – as per the ‘patient guide to level of vaginal bleeding’ as below, please call 999 as this may indicate you require urgent medical attention.
- If you are struggling with pain/heavy vaginal bleeding we advise that you contact the Early Pregnancy Unit or NHS 111 or call 999 in a medical emergency situation.
Unfortunately, nothing can be done to stop a pregnancy loss once it has started and this can be unpredictable. The nursing team will explain the different management options available to you, including expectant management, medical and surgical management.
It may be useful to be prepared for what the pregnancy may look like so you/your partner can make decisions relating to how best you can be supported and what you may wish to do with the pregnancy afterwards. We can guide and support you with this and this will be tailored to each individual’s personal choice/circumstance.
In the first month of pregnancy, the developing embryo is the size of a grain of rice so it is very difficult to see. You may pass a blood clot or several clots from your vagina. You may also pass some white/grey tissue in the clots. The vaginal bleeding can last up to 2 weeks.
At 6 weeks most women usually can’t see anything recognisable when they experience a miscarriage. The embryo is approximately the size of a fingernail. During the vaginal bleeding you may see clots, a small sac and a placenta.
At 8 weeks the embryo is the size of a small bean and you may be able to visualise the eyes and limbs. You may also pass tissue that is dark red in colour.
At 10 weeks the blood clots passed are dark red and can resemble ‘jelly’. The sac is likely to be inside one of the clots. The developing foetus will be very small but fully formed and may or may not be seen.
At 12 to 16 weeks you may first notice fluid leaking from your vagina followed by some bleeding and clots. The foetus will be fully formed and may be seen outside/ attached to the sac.
Options of how you wish to sensitively dispose of your pregnancy can be discussed with you by the nursing team. We understand this is a very distressing time for you and we will guide you through these options. We have various charities and a chaplaincy team at the hospital who can also support you and your partner/family (please see details at the end of this leaflet). If you wish to bring your pregnancy to the hospital so we can arrange a shared cremation you can use the pack (optional) supplied by the hospital. The pregnancy can be placed into the container provided along with the saline solution and returned to the hospital. Please contact the hospital on the contact numbers provided to arrange this. You will also be given the option to arrange a private funeral with a funeral director or a home burial. More information regarding these decisions will be provided to you by the hospital.
Pregnancy hormones will begin to fall after your pregnancy loss. This happens at different rates for different people. Once the bleeding stops, your hormones should gradually return to normal.
You may be asked to do a pregnancy test after 3 weeks to make sure this is happening (this can be provided by the hospital). If it is still positive, it is important you contact the Early Pregnancy Assessment Unit if this is the case. Depending on your symptoms you may be asked to attend the unit for assessment or to repeat the pregnancy test. Failure to do this may put you at an increased risk of an infection.
Your other pregnancy symptoms, such as feeling sick or breast tenderness, will also fade away.
As well as the sadness you may feel about what is happening, this change in hormone levels can also affect your emotions. You may feel very tired, get upset very easily or experience mood swings. Some women also experience breathlessness, anxiety and sleep problems, including difficulties going to sleep or sleeping a lot.
It is therefore really important that you seek help from your family/ friends/health professionals/ pregnancy loss support charities (please see details at the bottom of this leaflet).
If you normally have regular periods, your next period will usually happen around 4 to 8 weeks after a pregnancy loss. It may take several months to settle into a regular cycle.
You will ovulate before then, so you may be fertile in the first month after a miscarriage. You should avoid having sex until all your miscarriage symptoms have gone and a negative pregnancy test. This is to reduce the risk of infection and to avoid confusion between a new pregnancy or an incomplete miscarriage.
If you have experienced 3 or more miscarriages, there is an option for cytogenetic testing. A process whereby the pregnancy tissue is tested to look for changes in chromosomes. If you require further information regarding this, this can be discussed with the medical team responsible for your care in the Early Pregnancy Assessment Unit.
There is no right or wrong way to feel about pregnancy loss. Everyone is different. The list below gives you details of the agencies/charities available to you:
- Chasing Rainbow www.chasingrainbowscharity.com
- House of Light – Perinatal Mental Health Service | Support and Information | House of Light Email: help@houseoflight.org.uk. Tel: 01482 580499 or tel: 0800 0432031.
- Let’s Talk (Residents of Hull who are registered with a Hull GP) www.letstalkhull.co.uk – tel: 01482 247111.
- East Riding Talking Therapies (Residents of East Riding who are registered with an East Riding GP) – NHS East Riding Talking Therapies – tel: 01482 335451.
- Abbie’s Fund – Abbie’s Fund – Memory Boxes for Hull Women and Children’s Hospital
- Miscarriage Association – www.miscarriageassociation.org.uk
- Chaplaincy Service – tel: 01482 675966.
- Tommy’s – tommys.org
- Ectopic Pregnancy Trust ectopic.org.uk
There is an option for families to take a memory box home (these are available in the Early Pregnancy Assessment Unit). Please ask a member of staff if you would like to take one home with you.
You may wish to request ‘A baby loss certificate’. These are available at: http://www.gov.uk/request-baby-loss-certificate – tel: 0300 330 9445 or email: babylosscertificate@nhsbsa.nhs.uk.
Patient guide to level of vaginal bleeding