- Reference Number: HEY007/2023
- Departments: Paediatrics
- Last Updated: 31 August 2023
Introduction
This leaflet has been produced to give you general information. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is a Pressure Ulcer?
Pressure ulcers are areas of damage to the skin and under lying tissue. A pressure ulcer can vary from a red mark to a deeper wound depending how severe it is. How quickly pressure ulcers can develop will vary from child to child. People of all ages (from babies to the elderly) can develop pressure ulcers.
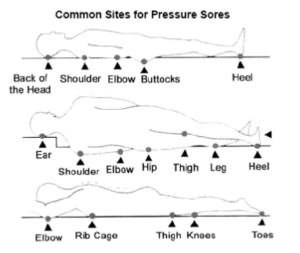
Diagram from ‘A Patient/Carers Guide to Skin Care’ – Permission given from the Tissue Viability Society
The 3 main causes of Pressure Ulcers are:
- Prolonged pressure to an area of skin, therefore if your child in is one position for a long time.
- Friction (rubbing) which can cause damage to the internal layers of the skin and tissue.
- Pulling your child across a surface can cause a shearing effect, which may make your child’s skin sore or split.
What can put my child more at risk of developing a Pressure Ulcer?
- Due to a disability that does not allow the child to move.
- It may be due to how ill your child is.
- Sedation (medicine to make them sleep).
- If the child cannot feel parts of their body i.e. legs or feet.
- If your child regularly wets or soils themselves.
- If your child has skin that is already broken or swollen.
- Under/overweight.
- If your child has had a long operation.
- If you child wears plaster casts or splints.
- If your child lies on the monitor leads, lines or if saturation probe sites are not changed regularly.
- If your child has a reduced immune system, has a high temperature or on long term steroids.
How Can I Reduce the Risk?
- Encourage your child to change their position regularly if safe to do so following advice from your nurse.
- If your child needs help to move then they may need specialist equipment to move them safety.
- Keep your child’s skin clean and dry.
- Signs to look out for are; red marks on the child’s body, sometimes purple / bluish in colour. Swelling, blisters, shiny areas, hot areas dry patches, cracked or wrinkled skin. If you notice any of the above on your child’s body report it to your nurse.
- The nurse may apply a clear film dressing to red areas on your child to add an extra layer to help prevent further damage.
- The nurse will reposition any monitor leads, lines or probes as often as necessary.
- We try to add additional padding to all splints and plasters in order to try and protect these vulnerable places.
- The dietitian can be contacted for dietary advice.
- All patients within our hospital are provided with good quality pressure reducing foam mattresses as a basic requirement of pressure ulcer prevention. If your child is identified as starting to develop a pressure ulcer they will be assessed by the ward nurse to decide if they require a special dynamic (air) mattress. This may be provided in order to help reduce or relieve any pressure. If this is appropriate for your child it will be explained to you.
- The nurses caring for your child will also assess your child’s skin regularly using an assessment tool called the Northampton Score.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Paediatric Departments on 01482 67040 or Acorn Ward on 01482 602703 or Woodland Ward on 01482 674465.
Useful contacts:
The Tissue Viability Society: societyoftissueviability.org
NHS Direct – Tel: 111
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats your child, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to your child. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your child’s condition, the alternatives available for your child, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about your child
We collect and use your child’s information to provide your child with care and treatment. As part of your child’s care, information about your child will be shared between members of a healthcare team, some of whom you may not meet. Your child’s information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide your child with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your child’s doctor, or the person caring for your child.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about your child. For further information visit the following page: Confidential Information about You.
If you need information about your child’s (or a child you care for) health and wellbeing and their care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.
