- Reference Number: HEY070/2020
- Departments: Radiotherapy
- Last Updated: 30 November 2020
Introduction
This leaflet has been produced to give you general information about radiotherapy to the lung(s). Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the health care team.
What is radiotherapy?
Radiotherapy is the use of high energy X-rays to treat cancer. Radiotherapy works by causing chemical and physical damage to the cancer cells in the treatment area. Although some normal healthy cells are also affected, these are able to recover and repair themselves.
Radiotherapy has a number of different benefits, like curing some cancers after surgery for example, but also may be used as symptom control. Radiotherapy is painless, does not make you radioactive and you are safe to be around people including children whilst you are having treatment.
There are different types of treatment. Your doctor will prescribe the most suitable type for you and explain the reason that radiotherapy has been recommended. You may also be having chemotherapy in combination with your radiotherapy and this process and its side effects will be discussed with you with your consultant and the chemotherapy team.
Your doctor will tell you how many treatments you will be having. The treatments are once a day and the appointments take approximately 20 to 30minutes. There is no special preparation for treatment but comfortable clothing is advised.
They will have already discussed the treatment, side effects and gained consent from you to receive your radiotherapy. There are several stages prior to you actually commencing your treatment.
Radiotherapy is delivered using a machine called a Linear Accelerator, or Linac for short. The picture shows the two different types of linear accelerators we have within our department.
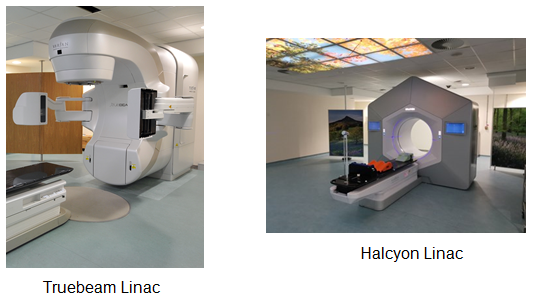
Images provided by the Radiotherapy Department at Castle Hill Hospital.
What will happen first?
Radiotherapy is designed individually for each patient so before you can start we will need to plan your treatment. This may mean a visit to our CT scanner to plan your treatment. This will all be carried out at the Queen’s Centre at Castle Hill Hospital. See leaflet ‘Introduction to Radiotherapy CT Planning’.
For this scan, you will be laid on a piece of equipment known as an ‘immobilisation board’ (Fig 1). You will be required to lay flat on your back with your arms raised above your head (Fig 2).
It is important that you are comfortable as this will be the position you will be in for your daily treatment. If you are not comfortable, please inform a member of staff at the time so adjustments may be made for your comfort.
For your CT planning and treatment appointments, your upper body will need to be exposed from the waist up. You will be provided with upper body treatment gowns for your convenience but the garment will also have to be opened for treatment.
Permanent Skin Marks
During the initial planning appointment pen marks will be drawn onto your skin, to ‘mark on’ the treatment site. As these pen marks will wash off, we prefer to make very small permanent skin marks before you leave the department. These permanent marks are made using a very fine needle and tattooing ink, and provide a permanent mark that we can use for reference when delivering your radiotherapy treatment. These permanent marks mean you are able to bathe and shower during treatment as normal.
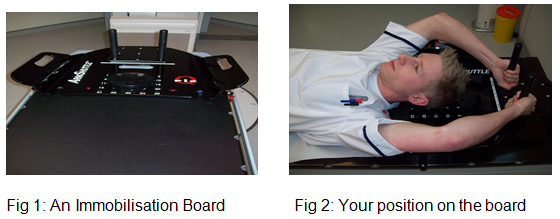
Image provided by the Radiotherapy Department at Castle Hill Hospital.
What happens during my treatment?
A member of staff will escort you into the treatment room. The treatment machines and rooms are very large and can appear quite overwhelming when you see them for the first time. You will need to undress to the waist (as for your planning scan) unless you are wearing an upper body treatment gown. There is a curtained changing area within the treatment room should you wish to use it and there are changing cubicles adjacent to each machine.
The therapeutic radiographers will then assist you into the correct treatment position on the couch. This is the same position that you were placed on the immobilisation board during your planning appointment. It will be necessary to open your upper body treatment gown at this point, if you are wearing one, to allow the radiographers to see your ‘permanent skin marks’. The radiographers will move you closer to the machine and will start to move you back into the exact position you were in for your planning scan, using the permanent marks.
They will then move the machine around you but it will not touch you. Once the machine is in the correct position the radiographers will leave the room but will be just outside the room watching you on a television monitor. This image is not recorded or stored; it is purely for patient safety. You will not see or feel anything apart from the couch and machine being moved into position and a buzzing noise while the radiotherapy is given.
Review appointments during treatment
You will have regular weekly reviews with a therapeutic radiographer as you progress through your treatment. This is to assess your general health and how you are coping with any side effects, so please be honest in your answers as this will be documented as an assessment of your treatment. You may be referred to one of our support team if further medical advice or intervention is required. Please do not feel this is the only time you can voice any concerns regarding your health, the therapeutic radiographers will ask how you are feeling every day before treatment.
What are the side effects of radiotherapy?
The side effects depend on the area being treated and the dose of radiotherapy you receive. The side effects should be discussed by the doctor with you before you consent to have your radiotherapy.
This is a general guide to the type of symptoms you may experience and how to deal with the side effects. If you are not sure how your radiotherapy may affect you or what to do if you need help, please ask your doctor, radiographers or nurses.
Skin
Your skin within the treated area may become pink and itchy. To help your skin feel better you should wash the area gently. Use a soft towel to pat the area dry, DO NOT rub. If your skin becomes more sore you may be given creams by the radiotherapy staff and told how often and how to use them. Use only creams given/advised to you by the radiographers or radiotherapy nurses. Skin reactions can get worse for a week or two after the radiotherapy is finished and you should continue to follow the advice given. The treatment area will be sensitive to the sun during treatment and also in the future, so please keep the area covered and use a high factor sun cream, at least factor 25 after treatment has finished.
Fatigue / tiredness
Radiotherapy can make you feel tired so it is important to rest as much as you feel you need to but still maintain gentle exercise. It is also important to drink plenty of fluids, more than you would usually drink. It does not matter what the fluid is but we do not recommend alcohol. If you are unsure please ask one of the radiographers or nurses within the department.
Nausea
Radiotherapy may make you feel nauseous (feeling sick). If this occurs, please inform the radiographers for advice or they may arrange for you to see a doctor. The doctor may prescribe some medication. If you do not feel like eating, try to drink plenty of fluids and report this to your radiotherapy treatment staff.
Discomfort on swallowing
You may find that you develop a sore throat or difficulty in swallowing. If your throat is sore while you are coming for your treatment, please tell the radiographers treating you as medicine can be prescribed to help. If your treatment has finished, contact your Clinical Nurse Specialist or GP for advice. Eating softer foods may help and also avoiding foods that are hot, cold, or spicy. If you do not feel like eating, try and drink plenty.
Cough
Radiotherapy to the chest and lungs can cause a cough; this may be productive (producing phlegm). If the cough becomes troublesome, please inform a member of your radiotherapy team or your Clinical Nurse Specialist.
Shortness of breath
Sometimes radiotherapy to the chest can cause inflammation in the lungs, which can feel like a chest infection with shortness of breath, cough and sometimes a fever. If this occurs during your course of radiotherapy please inform the treatment staff as you may need medication to help you. If you have finished your treatment please contact your GP for an urgent appointment.
All these side effects are general but if you have any worries or concerns please speak to a member of your radiotherapy team.
What happens after my radiotherapy has finished?
A follow up appointment will be made on your last day of treatment. It will be in a few weeks following the end of your radiotherapy treatment. If the appointment is made at the Queen’s Centre you will have the appointment details given to you before you leave. If the appointment is made at another hospital it will be sent in the post.
Research
Hull University Teaching Hospitals NHS Trust is a research-active Trust with a research strategy that includes cancer treatment and care. The radiotherapy department participates in national and international research studies to improve treatments to make them safer, more effective and to reduce side effects. We also develop patient-centred local research to improve your radiotherapy experience to benefit you and your family. We would like to encourage you to feedback about your experiences and ideas to help us to research the areas that are important to you. Your treatment will not be affected in any way should you not wish to take part.
Pregnancy
It is advisable that women do not become pregnant while having cancer treatment because the radiotherapy can have an effect on the unborn child. It is suggested that you use a barrier form of contraception (e.g. condoms). Please do not hesitate to ask your doctor or a member of the healthcare team if you have any questions or concerns about these issues.
Smoking
Stopping smoking during and after radiotherapy is very worthwhile. Research has shown that smoking may make the radiotherapy side effects worse.
Clinical Oncologist/Consultant Radiographer
These are specialists who are experts in radiotherapy and will be managing your treatment. They will take the responsibility for deciding what dose and how many treatments will be best for you; they will oversee the planning of your treatment.
Therapeutic Radiographers
Radiotherapy is delivered by male and female therapeutic radiographers who are specialist healthcare professionals that are trained to plan and deliver radiotherapy treatment and to the specialist equipment. They are there to help you if you have any problems or worries, please speak to them for any help and advice. They may refer you to a member of the Radiotherapy support team as necessary.
Radiotherapy Support Team
The team consists of Radiotherapy Nurse Practitioners, experienced Registered Nurses and Clinical Support Workers (CSW), who are based within the Radiotherapy Department who actively support and advise patients and their families may have relating to their radiotherapy treatment. They are able to make appropriate referrals.
Students
At some point during your treatment you may encounter student radiographers. Everything they do is supervised fully. If you would prefer our students not to be present during the planning and treatment please let a member of staff know when you attend for your initial planning appointment.
Contact information:
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Radiotherapy Information and Support Team on telephone number tel: 01482 461206, or email: hyp-tr.radiotherapy.information@nhs.net
Please note below the contact details of useful organisations that provide information about cancer including radiotherapy treatments:
Macmillan Cancer Support
Provides information from specialist nurses on all aspects of cancer and its treatment, and on the practical and emotional aspects of living with cancer.
Free phone help line: tel: 0800 8001234 (Monday to Friday, 9.00am to 8.00pm).
Online: www.macmillan.org.uk.
Write to: 3 Bath Place, Rivington Street, London, EC2A 3JR.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

