- Reference Number: HEY1439/2024
- Departments: Dietetics, Nutrition Support
- Last Updated: 30 November 2024
What is constipation?
Constipation is when you open your bowels (poo) less than usual or you are having a difficult time trying to push out a bowel motion (poo).
What are the signs and symptoms of constipation?
You may notice that your bowel motions become very large, hard, dry or lumpy. A normal bowel motion is one that is smooth and easy to pass.
Why do I have constipation?
There are many reasons why someone with kidney disease can develop constipation and these can include:
- Dietary changes and poor fibre intake
- Fluid restrictions
- Reduced activity or mobility
- Ignoring the urge to go the toilet
- Other medical conditions such as an under active thyroid, irritable bowel syndrome, etc.
- Some medications such as certain pain killers such as codeine or morphine or certain medications needed when on dialysis
- Stress, anxiety or low mood
Why is it important to avoid constipation?
If you are regularly pushing hard to have a bowel motion then you are more likely to develop haemorrhoids (piles) which can cause itching, pain and bleeding.
You may start having loose or watery stools after a few days of hardly moving your bowels at all. This does not mean that you are having diarrhoea. It may mean you are so plugged up that you are pushing loose or watery stools around a blockage. This is known as overflow diarrhoea.
Constipation can make you feel unwell and affect some of your blood results.
If you are having peritoneal dialysis (PD), constipation can squash your PD tube or cause your PD tube to move and make it difficult for you to drain out dialysis fluid. In extreme cases it can be a reason to stop peritoneal dialysis and move to haemodialysis. For those having automated peritoneal dialysis (overnight) then you are more likely to experience ‘drain pain’ when the dialysis fluid is being drained from your abdomen.
How can constipation be treated?
Prevention is better than cure so it is best to avoid becoming constipated in the first place. This can be done by:
Improving your toilet routine
- Do not delay if you feel the urge to poo.
- Keep to a regular time and place and give yourself plenty of time to use the toilet.
- To make it easier to poo, try resting your feet on a low stool while going to the toilet.

Diet and lifestyle changes
Regular bowel movements can be achieved by following a high fibre diet. Some people will also need medications to help to ensure regular bowel movements e.g., Hyfiber (fibre supplement), senna, docusate sodium or laxido (laxatives) prescribed by your doctor.
To keep your bowels healthy it is important to:
- Follow a high fibre diet – include some high fibre foods at each meal.
- Eat regularly – avoid skipping meals.
- Make sure you have your full fluid allowance.
- Exercise regularly as able.
How much fibre do I need?
For adults in the UK, dietary fibre intake should be 30g a day as part of a healthy balanced diet.
There are two types of fibre:
- Soluble fibre – found in foods such as oats, fruit, vegetables and pulses e.g. peas, beans, lentils.
- Insoluble fibre – found in foods such as wholemeal bread, wholegrain cereals, jacket potatoes and brown rice.
Try to have both types of fibre daily to prevent constipation. If your intake is low, fibre should be introduced gradually to allow your body to adjust. Discuss this with your dietitian.
How to eat more fibre
- Have a high-fibre cereal at breakfast e.g. Weetabix, Porridge Oats, Shredded Wheat and add some fruit e.g. raspberries, blueberries or stewed apple.
- Have an oat-based cereal bar as a snack (check the label and be aware of sugar content).
- If you are having a biscuit choose those that are higher in fibre e.g. whole wheat biscuits, digestive biscuits, brown and whole wheat crisp breads.
- Add linseeds to yogurt or salad or add to a glass of warm water. Start by adding 1 teaspoon of linseeds each day, you can increase to 1 tablespoon if required.
- Choose wholemeal, granary or ‘best of both’ bread and bread products.
- Choose wholemeal or brown rice and pasta.
- Try a homemade vegetable or lentil soup with wholemeal/rye bread.
- Add peas, beans or lentils to dishes, these are a healthy, nutritious and cost effective way to bulk up stews, casseroles and curries.
- Have more meals based around beans, lentils and pulses rather than meat/chicken or fish e.g. three bean chilli, bean burgers or chickpea curry.
- Add extra vegetables to sauces such as Bolognese, curry and chilli.
- Leave the skin on fruit and vegetables and aim for 5 portions daily. If you are following a low potassium diet then choose lower potassium options and consider cooking methods.
Note: a portion of fruit and vegetables weighs 80 grams (3 ounces) which would be a handful of small fruit (strawberries, raspberries, grapes etc.) or one small apple, peach or tangerine or 3 heaped tablespoons of vegetables or a small bowl of salad.
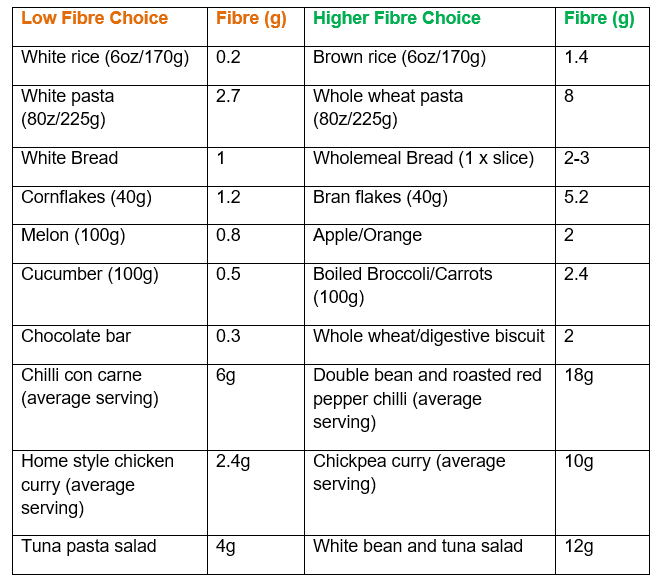
Examples of high fibre dietary swaps
Below is a sample menu on how you can include 30 grams of fibre per day:
| Portion Size | Fibre | |
| Breakfast | 2 shredded wheat | 5.5g |
| 80g strawberries | 3g | |
| Snack | 1 medium pear | 3g |
| Lunch | 2 x slices wholemeal bread sandwich with tuna and salad | 7g |
| Multigrain snacks 25g bag | 2g | |
| Evening meal | Chicken, leek and brown rice stir fry | 7g |
| Snack | 30 grams of unsalted almonds | 3g |
Should you require further advice, please do not hesitate to contact the Dietetics Department on tel: 01482 674490

