- Reference Number: HEY1520/2025
- Departments: Cardiology
- Last Updated: 31 January 2025
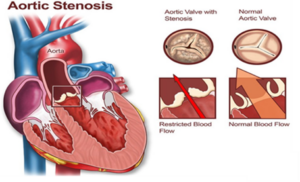
Your doctors are treating you for a condition called aortic stenosis. This is when the main valve (aortic valve) which allows blood to flow from the heart to the rest of the body become narrowed, thus restricting blood flow.
What causes Aortic Stenosis?
In most cases, aortic stenosis is due to general wear and tear and is more common as we age. In some cases, the valve has been abnormal since birth and has become more narrowed or leaky over time. The valve may also become abnormal due to other conditions such as rheumatic fever.
What are the symptoms of Aortic Stenosis?
Aortic stenosis may cause symptoms of chest discomfort, breathlessness, or blackouts. As the valve narrowing worsens, this can cause weakening of the heart muscles pumping action (known as heart failure) and this may become a life-threatening problem over time.
Can Aortic Stenosis be treated?
If the aortic valve is not severely narrowed, no specific treatment is needed. You will be offered routine check-up appointments to monitor the valve for further deterioration and assess your symptoms.
If your heart valve is severely narrowed, you may be suitable for a number of treatment options. Before deciding which treatment is best for you, several tests will need to be completed.
Routine tests include:
- Blood tests
- An ECG (electrical trace the heart)
- An echocardiogram (ultrasound scan of the heart)
- A detailed CT scan of the heart and blood vessels
- A coronary angiogram – passing a tube into your wrist or groin arteries to assess your coronary (heart) arteries
In some cases, more tests are needed may include:
- Transoesophageal echocardiogram (TOE). This is a more detailed ultrasound scan of the heart where you asked to swallow thin tube which shoots a look at the heart failure gullet.
- Lung function tests (breathing tests by blowing into a small tube).
Treatment Options
Trans-catheter aortic valve implantation (TAVI)
During this procedure, the patient’s own valve is not removed but is squashed by a tissue valve which is held in place by metal frame. In TAVI, the new valve is inserted from the blood vessels in the groin or by a small cut in the upper chest wall (other access sites can be used, if needed these will be discussed with you). The heart does not need to be stopped, and a bypass machine is not routinely used. The procedure is performed under local anaesthetic – meaning you are awake for the procedure. Mild sedation may be used, especially if you are anxious prior to the procedure.
Open heart surgery
During surgery, the narrowed valve is removed and replaced with an artificial valve. You will have a general anaesthetic, and you will be asleep for the operation. To do this, a cut is made through the breastbone to open the chest and reach the heart. The heart is then stopped artificially to allow the valve operation to take place. During the operation, a bypass machine is used to pump blood around the body.
Medical treatment
The third possibility for management of aortic stenosis is medication alone. This is more to alleviate symptoms, especially with diuretics (water tablets) or other tablets to help the heart pumping action. It is however important to bear in mind that medical treatment alone would not alleviate all your symptoms and carries substantial risk of death.
How will I know which treatment is best for me?
All patients are discussed at a multidisciplinary team meeting (sometime known as MDT, MDM, or Heart Team Meeting), where cardiologists, cardiac surgeons, specialist nurses, and in some cases cardiac anaesthetist will be present. Your case and investigations will be discussed, and appropriate treatment options will be recommended.
What happens next?
Once your case been discussed, we will recommend a treatment plan for you. We will make an appointment either face to face or via the telephone to discuss the treatment option with you in more detail. If valve intervention treatment is not recommended, we will inform you and your doctor. Where both surgery or TAVI treatment options are considered appropriate, you will be invited to meet both the surgical and TAVI teams to explore your options and preferences.
TAVI
If you are suitable for the TAVI procedure, we will add you to our waiting list once all investigations are completed. The telephone numbers at the end of this booklet should be used if you become unwell before you have your TAVI.
Pre-admission Clinic
You will be seen in pre-admission clinic prior to your procedure. This appointment will normally last for up to 2 hours.
Where possible we would recommend that you bring a member of your family or close friend to the appointment with you.
During this appointment we will discuss your procedure in more detail and answer any questions you may have. We will review your symptoms, medical history and may perform a physical examination. Blood tests and a heart tracing will be performed as final checks before you come into hospital.
How is TAVI performed?
In most cases this will be performed via the groin arteries (referred to as trans-femoral access) or through the arteries under the collarbone (called the subclavian artery). During TAVI, the new valve is held in place by the surrounding tissues and your old valve is not removed. At the end of the procedure, we will do a number of checks to ensure that your new valve is working properly. We use a number of different TAVI valve types. The team looking after you will select the preferred TAVI valve type and size based on the scans you have already had.
Transfemoral TAVI
Transfemoral TAVI is usually done under local anaesthesia, which meaning you will be awake and able to talk to the team during the procedure. Small doses of certain sedatives or painkillers can be used to minimise discomfort.
Occasionally, we may need to convert to a general anaesthetic if you are finding the procedure difficult to tolerate. This will however increase your procedural risks.
Small skin incision is made in the groins so that we can insert the equipment. We will also often need to use your other leg and at least one of the arteries in your arm for other smaller tubes to guide the procedure. A catheter (tube) will then be passed through the blood vessels with your new valve attached. Once in the correct position your new valve will be deployed.
The small hole is closed at the end of the procedure using internal stitches or other closure devices. The small internal stitches or plug do not need to be removed later.
IN THE CATH LAB
- You will need to lay flat for the procedure. You can have one pillow, but it is important to keep still.
- Pain – you may be given intravenous paracetamol at the start of the procedure. There may be times when passing the tube, the pain is worse, but you will be able to have strong painkillers if necessary. You must say if the pain is too much.
- Valve deployment -for the valve to be deployed we will use a pacing wire to make the heartbeat extremely fast and the blood pressure to be lowered to stop the valve from being moved. This may make you feel unwell and dizzy and may even pass out briefly. Be reassured that it is a controlled environment and can quickly be reversed.
POST CARE
- You will need to be on flat bed rest for at least 2-4 hours, Then, if groin sites are ok, you will be allowed to sit up at 45 degrees. Should be mobile after 4 hrs. We aim for you to start mobilising after 4 hours if all goes well.
- Your Heart rate needs to be monitored for at least 24 hours. If you have an existing pacemaker, you may go home sooner.
- Discharge will depend on how the wound sites heal and heart rate and rhythm
Subclavian approach TAVI
If the groin arteries are too small or narrowed, the procedure may be done through the arteries running under the collarbone (called the subclavian artery). This approach requires a general anaesthetic. An incision is made in the skin in the upper chest by a surgeon. A catheter (tube) will then be inserted which will allow us to pass your new valve to your heart.
The incision is closed at the end of the procedure with sutures. The general anaesthetic will be stopped, and you will gradually wake, either in the Cath lab or in a recovery area.
Other access
Other access site may be used in some cases. If these are to be used, they will be discussed in detail with you by your doctor or nurse.
What are the benefits of the procedure?
A successful procedure relieves the narrowed valve and improves the overall heart function. This will usually improve symptoms of chest pain, breathlessness, and blackouts.
This may improve your overall quality of life and your life expectancy.
What are the risks of the procedure?
With any procedure there are risks of complications. However, there are also risks from leaving the valve untreated. Your doctor will weigh up the risks and benefits carefully with you as the risks we quote can vary according to your medical history and clinical condition (the risks quoted below are national averages for the UK where available).
Major and/or common risks (can occur during or after the procedure) include:
- Death – 2%
- Bleeding or damage to the blood vessels needing further surgery or blood transfusion – 4%
- Stroke or mini-stroke (TIA) – 2 to 3%
- Heart attack – 1%
- Permanent pacemaker insertion because of slow heartbeat – 10% (depending on your ECG at baseline and the valve type used)
- Emergency open-heart surgery (not every patient is suitable for this, and this will be discussed with you prior) <1%
Serious risks include:
- Bleeding into the sack around the heart – 1%
- Reaction to dye – <1%
- Kidney failure – <1%
- Infection of the heart valve – <1% long-term risk
Less serious risks include:
- Valve leak – a small amount of leak around the new valve is common but significant leak occurs in 2 to 3% of cases.
- Conversion to a general anaesthetic
- Abnormal heartbeat
- Bruising around the wound
- Failure to insert a new valve
Occasionally patients may become confused or disorientated after the TAVI procedure. This may be related to the procedure itself or the patient’s general health in combination with a stay in hospital. It commonly settles in a day or so but rarely, can be more prolonged.
Dental care before TAVI
It is essential to maintain healthy gums and teeth especially if you have heart valve disease. This is to reduce the risk of dangerous infection of the heart valves, known as endocarditis.
It is important that you have dental checks before your heart valve procedure. It may be recommended that dental treatment is necessary, and this may need to be carried out before TAVI is performed. Please register to a dental practice if you do not see a dentist regularly.
What happens after the procedure?
After the procedure, you will be transferred to either the day unit, cardiology ward or coronary care unit, where your heartbeat will be monitored. Rarely, patients may need to attend the intensive care unit. On most occasions, all the tubes inserted during the procedure will be removed. You may be able to sit up or walk quite quickly after the procedure, but sometimes this can take a little more time depending on your recovery If tubes are left in, we will explain why.
Whilst in hospital, you will have further ECGs and blood tests. The need for any extra tests will be decided by your doctor. This will be discussed with you.
If your progress is uncomplicated, you may be discharged the following day after the procedure. This will be discussed with you when you attend the pre-admission clinic. The duration of stay in hospital can sometimes be longer if your recovery is slower.
- Physical Activity; you should avoid any strenuous activity for 4 weeks following your procedure. You may feel drained for a few weeks after the procedure but should aim to go for a short walk each day, which can gradually be increased throughout your recovery.
Your specialist nurse will discuss your activity if alternate access was used.
- Wound Care; your wounds should only be small, so they should be almost healed by the time you leave hospital. If you do still need a dressing, then it could be organized with either your district nurse or practice nurse to do this. You may also notice some bruising in your groin, which is normal. You may develop a hematoma, which is a hard lump under the skin due to a build-up of blood, and you should contact your GP if this gets bigger or painful.
- Medications; Some of your medications may be changed following your TAVI. If you are not already on blood thinning medications, you will be started on Aspirin.
Patient discharge after TAVI
Most people, upon discharge, feel an improvement in their symptoms. However, recovery continues at home, and you may need added support in the short term. The rate of recovery can vary from person to person.
You will be seen by the doctor and specialist nurse after the procedure and be given a discharge information advice leaflet about ongoing recovery.
You may will be referred to the cardiac rehabilitation service, who can aid you in returning to normal activities.
You will have an echocardiogram after the procedure and 6 weeks later as an outpatient. We will arrange a TAVI Nurse follow up telephone call within 8 weeks to discuss recovery and report echo results. If needed, we will arrange for you to come back to the hospital for face-to-face review. If you do not receive an appointment within 12 weeks of discharge from hospital, please contact the TAVI nurse on or tel: 01482 461516.
Driving
The DVLA recommends that you should not drive for 4 weeks after your procedure. You do not need to inform the DVLA about your procedure, but we do recommend you tell your insurance company to avoid any claims that you may make in the future. If you hold a commercial license you will need to inform the DVLA who will recommend you further.
Flying
Provided you have not experienced complications, you will be able to fly 1 week after if your TAVI was performed through your groin, or 2 weeks after your TAVI if you had a cut made in your chest. Regardless, if you are planning a holiday, it may be better to wait until your follow-up has been completed. If you wish to fly within 3 months of your procedure, check with your airline beforehand and you have valid travel insurance.
National audit and taking part in research
New medical or surgical procedures are subject to a great deal of investigation to find out ways of improving them, or to decide which patients they should be offered to.
You need to be aware that all TAVI cases in the UK are audited by the National Institute for Cardiovascular Outcomes Research (NICOR). It is a national requirement. This is for learning and monitoring purposes and your clinical information will be treated confidentially.
Additionally, the team at the Hull University Teaching Hospitals are involved with clinical research and you may be invited to take part in one. Your cardiologist or surgeon will discuss any potential studies in detail with you. It is important that you are aware that any such research involvement is strictly voluntary and that your care will in no way be affected if you decide not to take part. However, such research is valuable in improving care for patients in the future who may have similar problems to your own.
Where can I get more information?
- The British Heart Foundation website:
https://www.bhf.org.uk/informationsupport/treatments/tavi
- The National Institute of Clinical Excellence (NICE) website:
https://www.nice.org.uk/guidance/ipg586/informationforpublic
If you do not have access to the internet, your cardiologist can provide a copy of these documents.
- Your cardiologist or cardiac surgeon
If you require further information, please contact us:
Patient Experience
Hull University Teaching Hospitals NHS Trust would like your feedback. If you wish to share your experience about your care and treatment or on behalf of a patient, please contact The Patient Experience Department who will recommend you on how best to do this.
This service is based at Castle Hill Hospital but also treats patients from North and East Yorkshire and North Lincolnshire.
Should you need further advice on the issues contained in this leaflet, please do not hesitate to contact the TAVI Team on tel: 01482 461516

